
Next you will learn:
- What general complications after dental implants can await you on the way to restoring the ability to chew normally and smile beautifully;
- What problems sometimes arise immediately at the time of the operation, and which some days, weeks, months, and even years after the installation of implants;
- List of contraindications for implantation and their relationship with the development of dangerous complications;
- How can you recognize the problem in time - what is considered a harmless side effect and what is a dangerous complication;
- How to protect yourself as much as possible from possible troubles;
- What types of implants are characterized by the lowest risk of complications;
... And also other nuances of practical interest regarding possible complications of dental implants.
Unfortunately, a person’s permanent teeth, in the event of their loss or serious damage, are not able to recover on their own and require artificial replacement, since a violation of the chewing function not only causes significant damage to the digestive system, but also negatively affects the quality of life in general. In order to return aesthetics and normal chewing of food, dentists already in the late XVIII - early XIX centuries began to use the first, then still primitive, dental implants made of wood, various metals, porcelain and other available materials. However, the very frequent complications after dental implantation operations forced doctors to constantly look for new technologies and more advanced materials suitable as implants.
Thanks to such continuous research and successful experiments of doctors who are advocates of dental implantation, already at the end of the last century this direction in dentistry has become one of the most popular and in demand among the general population. The most important result of such hard work was that the complications after dental implants ceased to be regular and expected., and dental surgeons have learned to one degree or another to minimize damage to health, even in the event of certain problems.
Currently, implant prosthetics is gradually replacing the “conventional” prosthetics, often requiring healthy teeth to be sharpened, or using partial or full removable dentures, which are often called “false jaws”.
However, is it possible today, when the 21st century is already in the yard, to say with full confidence that the complications after dental implants and the corresponding risks of problems during and after the operation have already completely receded into the distant past? Well, the answer here is quite clear, and, unfortunately, is negative - complications are still often encountered in the practice of implantologists. But why?

In connection with the proliferation of numerous implant systems, various implantation techniques and technologies, as well as the training of many hundreds of practicing maxillofacial surgeons in our country alone, at least 20 thousand implants are installed per year. And at the same time, the number of unsuccessful operations and negative reviews on the Internet is quite naturally increasing - problems can begin through the fault of an insufficiently qualified doctor, due to the choice of poor-quality implants (rarely, but it happens), and also through the fault of the patient himself at the dental clinic.
About how to minimize the risk of problems during dental implants, how to avoid the most common problem with implants - their “rejection”, as well as what to do if problems are nevertheless outlined - we’ll talk about all this in more detail ...
Complications that may arise during the dental implantation procedure itself
It is useful to keep in mind that some complications may arise directly during the dental implantation procedure, right on the dental chair. Moreover, the nature of the undesirable consequences may depend on whether an implant is installed on the upper or lower jaw.
The following is a short list of possible complications that may arise during the implantation procedure (in decreasing order of frequency of occurrence):
- Severe bleeding;
- Pain;
- Perforation of the maxillary sinus and nasal cavity;
- Damage to the wall of the mandibular canal and nerves of the lower jaw.
Let's look at these complications in order.
Heavy bleeding
During tooth implantation, slight bleeding is considered normal, and in most cases it is easily eliminated by conventional hemostatic techniques. Excessive bleeding can occur both through the fault of the doctor, and through the fault of the patient himself.
The strength of each person sitting in a dental chair to reduce the risks of developing this complication. Most often, bleeding from a wound occurs with an increase in blood pressure, as well as in violation of blood coagulability (taking drugs that "thin the blood", cardiovascular pathology, etc.).
Blood pressure monitoring, timely administration of drugs under the supervision of a cardiologist or therapist, proper medication and psychotherapeutic sedative (stress-relieving) preparation, as well as mandatory informing the implant dentist about existing diseases will help to avoid not only early bleeding during implantation, but also in a delayed period. The implementation of all recommendations after dental implantation, when a fresh wound is a zone of increased attention, is also of great importance for the prevention of complications, especially if more than 4-5 dental implants were installed in one day.
From the practice of the dentist
Bleeding due to the dentist’s fault occurs much less often than most people think (after all, what kind of thoughts can the patient have: “Well, I’ve cut my entire jaw, now the blood doesn’t stop, couldn’t it be more accurate to cut it ...”)
However, doctors who are just starting their activities in the field of dental implants and stuffing the first bumps, do sometimes sometimes experience unpleasant flaws in their work. However, even if errors are made during the surgical operation, not even an experienced surgeon can easily use modern hemostatic techniques and means to eliminate the negative consequences. Only wounding large vessels deep in the jaw, for example, with an improperly selected implant, can pose a threat to the patient’s life, but this is very, very rare (almost impossible).
Pain during dental implantation
Sometimes during the dental implantation procedure, quite strong painful sensations can occur, which, however, are usually easy to eliminate with an additional portion of anesthesia.
But in rare cases, it happens that anesthesia works badly. This is most often associated with the individual characteristics of a person. This situation is resolved simply: dental implants are performed under general anesthesia, in other words, when consciousness is turned off.

Therefore, if you are injected with an anesthetic, but the pain is still felt, you do not need to endure and be silent - you should definitely and immediately tell the doctor about it.
Perforation of the maxillary sinus and nasal cavity
Currently, this complication of implantation is much less common than before. Progress was largely due to the ability to accurately determine the distance to the abdominal masses using panoramic images and computed tomography (CT).

In order to reduce the risk of this complication to almost zero, you need to trust only an experienced doctor with a long record of work, and in case of doubt - consult with other implantologists. In the case of a close location of the maxillary sinus and the bottom of the nasal cavity, a “build-up" of the bone (sinus lift) can be previously performed, and then there are no problems.
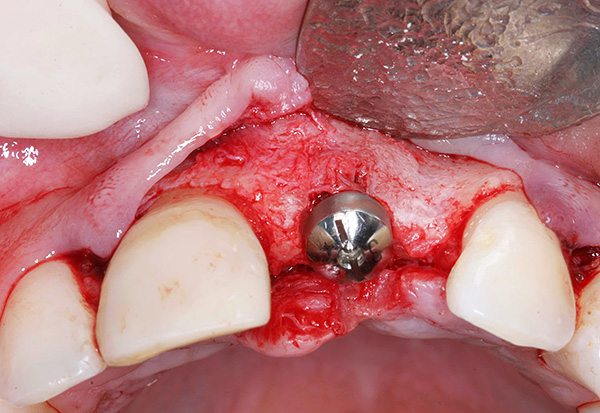
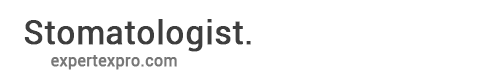
The photo below shows an example of bone tissue extension before tooth implantation:

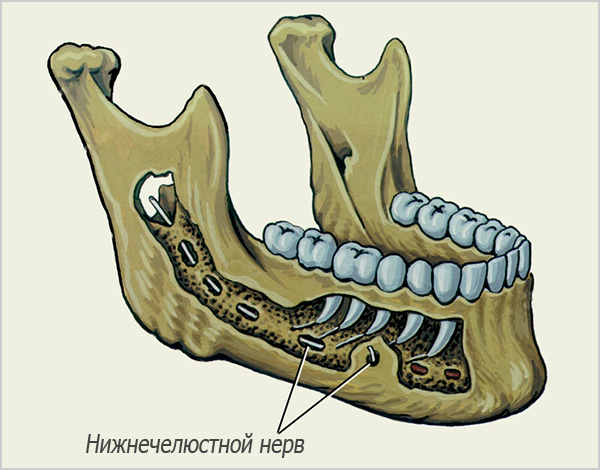
Damage to the wall of the mandibular canal and nerves of the lower jaw
This complication during dental implants does not always have long-term negative consequences, because, despite the frightening name, it actually manifests itself usually only as numbness in the lower jaw (most often the lips go numb). Even without treatment, these symptoms can disappear on their own within 2-3 weeks, with a maximum of 2-3 months.
In addition, it should be borne in mind that the feeling of numbness on the corresponding side of the face can also be a consequence of compression of the nerve in the mandibular canal. This sometimes occurs due to bleeding in the bone marrow spaces - blood can flow out not only towards the oral cavity, but also gradually move through the spaces of the bone, because the intraosseous tissue of the jaw is not “solid”, but cellular. The entry of even a relatively small amount of blood into the region of the passage of the mandibular nerve in the canal creates temporary compression. Gradually, the blood masses dissolve, but it takes time when the nerve recovers from such a compressive effect (usually no more than 5-7 days).
On a note
Complications such as a fracture of an instrument during surgery, a fracture of the wall of the alveolar bone, insufficient fixation of the implant, pushing it into the sinus of the upper jaw, etc., are even less common. The myth that a dental implant can get out of the eye or appear from the jaw through the cheek makes some people panicky about implantation. In fact, not a single doctor in his right mind will consciously harm your health using implants of the wrong length, and mindlessly screw them “all the way”. Therefore, this situation can be considered only from the point of view of popular horror films.
What complications sometimes arise after implant placement?
Complications after the installation of dental implants can be divided into the earliest, which manifest themselves within a few days after the operation, and later, arising in weeks, months, and sometimes years after implantation.

Early complications include:
- Painful sensations;
- Swelling;
- Bleeding
- Fever;
- Seam discrepancy.
Generally speaking, pain is a normal reaction of the body in response to the traumatic intervention of a dentist-surgeon during dental implantation, and such pain appears after the end of the action of anesthesia.
Analgesics prescribed by the doctor usually effectively relieve pain, and the engraftment process does not bring too much discomfort to the patient. Normally, pain should not bother for longer than 2-3 days, during which time medication is indicated. If the expressed pain lasts longer - this is an alarming sign.

Soft tissue edema is the result of almost any surgical operation, including dental implants. Moderately expressed edema is a natural reaction of the body to injuries and "invasion", in general, of a foreign implant, and rarely lead to complications. Usually swelling of the tissues lasts no more than 5-7 days.
A possible complication in the form of an excessive increase in edema can be prevented by applying cold immediately to the face area where the implants were placed immediately after the operation.In this case, you should be careful and follow basic common sense so as not to cause frostbite and tissue necrosis (that is, comrades who just take something ice from the freezer, put it on their cheek and hold it for two hours - this is wrong and very dangerous) .
Weak bleeding in the area of dental implant placement can be observed within a couple of hours after implantation, when the vasoconstrictor effect of adrenaline added to the anesthetic ends. Even if such bleeding is delayed for a whole day - this is not a cause for concern. It is important in this case to distinguish between the sacrum (bloody fluid) from the strong and ongoing bleeding for more than 5-8 hours, which does not stop.
Important:
It should be remembered that a common cause of bleeding is the inattention of the person himself to the existing problems. For example, taking aspirin and several other drugs worsen blood coagulation, and high blood pressure prevents the formation of a clot in the wound; a number of diseases of the cardiovascular system make ineffective almost all home methods of stopping bleeding. It is important to always timely and correctly assess the scale of the problem and notify your doctor in advance of such nuances.
As for a slight increase in body temperature after implantation, this is also a completely normal reaction, which reflects one or another stage of the local inflammatory process after surgery. On the first day, the temperature can rise even to 38.0 ° C, but do not worry - the problem is solved with the help of antipyretic drugs, which is likely to be mentioned by the doctor himself.
However, if, say, closer to night, the temperature on the first day after implantation "exceeded" far beyond 38 degrees, and antipyretic drugs do not help, then it is advisable to call an ambulance, make a lytic mixture, and consult your dentist in the morning, as this may be a sign of complications after dental implants.

Most often, the temperature does not rise to such high values, but can stay in the range of 37.0-37.3 ° C for several days, which is a reaction of the body that is within normal limits.
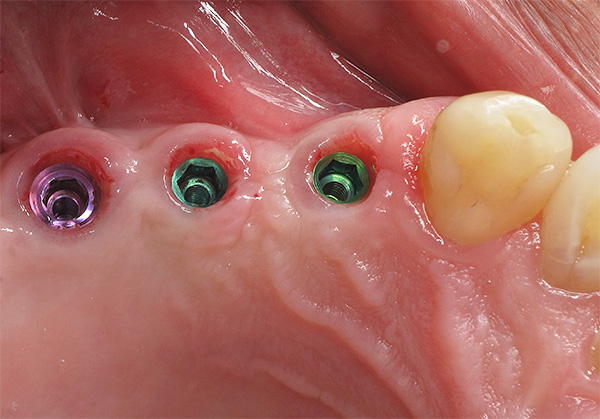
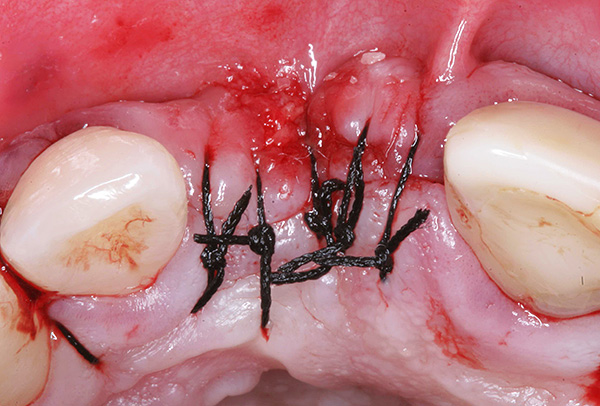
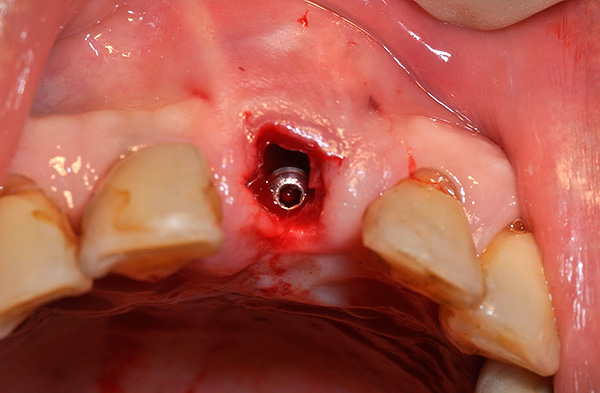
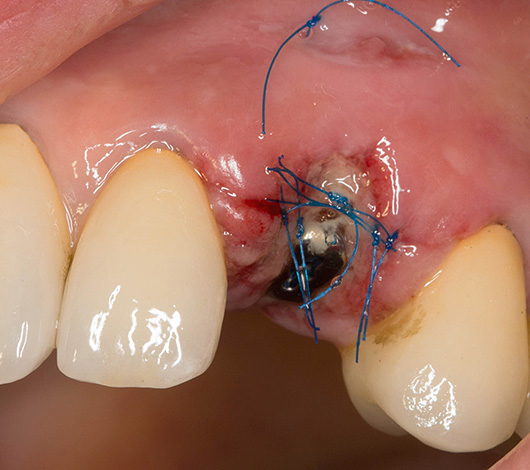
Perhaps, it is also worth mentioning the divergence of sutures, often applied to the wound after implantation. The photo below shows an example of the normal state of the sutures immediately after surgery:
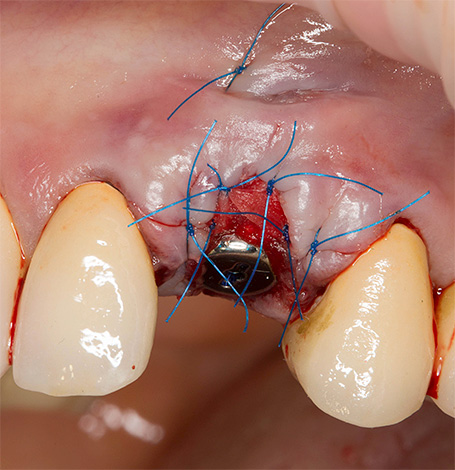
The divergence of sutures, as a complication, almost never is a sign of unsuccessful dental implants, since they more characterize the result of the behavior of the person himself. Violations can be very different: from non-observance of the principles of oral hygiene and ignoring the doctor’s recommendations, to unauthorized “tapping” in the oral cavity with fingers, toothpicks, etc., which leads either to mechanical damage to the sutures, or contributes to the onset of the inflammatory process. This provokes the divergence of seams in the future.
Late complications
Among the late complications that sometimes occur after a long period of time after dental implantation, the following can be distinguished:
- Periimplantitis;
- Implant rejection.
These complications can arise regardless of whether implants were installed on the upper or lower jaw, several or only one was placed, whether expensive implants were used or not. The risk of rejection and peri-implantitis (inflammation in the area of the implant) is always present, although, of course, quite certain factors influence the likelihood of such an unpleasant outcome.

Popular medical forums, which publish a lot of people's reviews on the results of dental implants, are often full of descriptions of various problems after seemingly successful implants. Moreover, violations associated with the "engraftment" of implants are usually among the first.
In fact, peri-implantitis and implant rejection are not as common today as one might think after reading the corresponding negative reviews. Each major clinic maintains official statistics on its unsuccessful cases, and the percentage of rejection from all registered implants is no more than 3-5%.
Moreover, often in such cases there are people who have been warned about the risks of rejection of dental implants in connection with existing contraindications, or who regularly violated recommendations for their care of prostheses on implants and had bad habits.
On a note
Periimplantitis is an inflammation of the tissues surrounding the implant. An infection that occurs when hygiene is not observed (most often), or if the implant installation technique is violated (extremely rare) can literally corrode the bone, leading to edema, suppuration, and severe pain. This complication is sometimes accompanied by the appearance of an unpleasant implant odor.
Further progression of peri-implantitis in case of failure to provide timely assistance leads to rejection of the implant - in such cases it is better to remove it immediately, without waiting until the inflammatory process leads to much more serious complications.
Rejection of the implant is often accompanied by its mobility and pain during exercise (when pressed). However, modern dentistry can sometimes solve even this, at first glance, the most terrible problem for many patients, a problem. However, we are not talking about the fact that the rejected implant will successfully take root after some manipulations by the doctor - no, it usually needs to be removed and re-implanted.
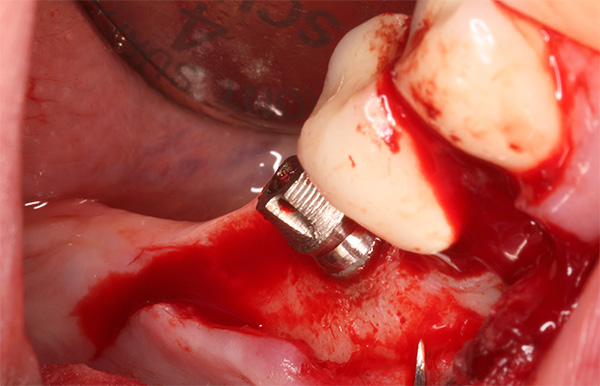
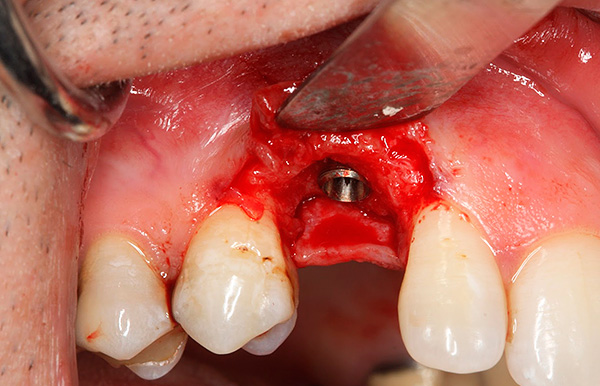
The photos below show the removed implants:


After removal of the movable implant, a complex preparation of the well for the next implantation is carried out, which can be carried out after 1-2 months. For example, with a significant decrease in bone tissue or proximity to the maxillary sinus, it may be necessary to build the jaw bone under the dental implant (sinus lift operation).
Indications and contraindications for dental implants and their relationship with possible complications
Indication for implantation is the absence of one or more teeth, as well as the impossibility of classical prosthetics. However, errors and complications when installing implants occur most often in those dentists who are guided to a greater degree by indications than by fully taking into account contraindications for implantation (sometimes this approach is due to commercial considerations, because no one wants to lose “expensive” patients).

Absolute contraindications for dental implantation:
- Chronic diseases in a decompensated stage;
- Severe hemostasis;
- HIV and a number of other seropositive infections;
- Some mental illnesses.
Relative contraindications:
- Diseases in the acute stage, especially acute viral infections;
- Chronic infectious diseases;
- Condition after a heart attack and stroke;
- Pregnancy and lactation;
- The risk of bacteremia in patients with prosthetic heart valves after rheumatism or endocarditis;
- Exacerbation of chronic forms of disease;
- Conducting treatment with drugs that worsen tissue regeneration.
Relative contraindications give the doctor the right to postpone the dental implantation procedure. For example: after a full cure of a viral disease, a year after a heart attack, after breastfeeding, cessation of drugs that create risks of complications during and after implantation, etc., All this is necessary to minimize the risks of developing negative consequences implantation of teeth.
It is interesting
More recently, diabetes was an absolute contraindication to dental implantation. But at the moment it is proved that type 2 diabetes mellitus in the compensation stage does not affect the course of implantation and does not create risks of implant rejection.However, the operation is carried out under the strict supervision of an endocrinologist with mandatory monitoring of blood glucose levels (significant fluctuations in glucose levels are unacceptable).
Some people who, by all means want to get a beautiful smile as soon as possible after dental implants, sometimes have reasonable questions:
- Or maybe you can still do dental implants during pregnancy?
- And during an acute infectious process?

So, simultaneous removal and implantation of teeth during pregnancy can in some cases have serious negative consequences for the fetus, and it is difficult to imagine a situation where surgery is simply urgently needed. Better still wait. Pregnancy itself does not affect the process of “engraftment” of implants, but drug therapy, which is necessary after their installation, can have a negative effect on the developing fetus.
Even in case of an emergency, for example, an acute injury, which led to a fracture of the tooth or root and its subsequent removal, during pregnancy you should not rush with implantation. It is clear that the aesthetic problem that a young girl has can lead to stress and a nervous breakdown, but the health of the unborn child should come first.
As for implantation in acute infectious processes - due to the action of the infection, the body is weakened, and there is an increased risk of peri-implantitis when installing implants at this time. However, this does not mean that it is impossible to place implants in the well of a tooth removed due to exacerbation of chronic periodontitis of the tooth. Adequate drug therapy, proper selection of the system and technology of implantation can, of course, minimize the risks of complications even in such extreme cases, although it is generally unreasonable and dangerous to neglect contraindications, especially when this is done by a doctor only for commercial gain.
How to recognize the problem in time: from harmless side effects to dangerous complications
Despite the associated risks, a huge number of people all over the world put implants, get a Hollywood smile and the ability to chew food normally. As for the possible complications - someone is more lucky, someone less, but the positive effect of implantation directly depends not only on the professionalism and intuition of the dental surgeon, but also on the patient himself.
The knowledge that allows you to recognize the problem in time and timely direct the situation to your advantage is not available to everyone. And if you rephrase a well-known saying, you get a kind of formula for a successful rehabilitation period after dental implantation: “Whoever owns the information knows the situation.”

Suspicious symptoms most often occur on the day of implantation or within 1-2 days after it.
Side effects can be observed even after jaw bone growth under the dental implant, which, however, does not always indicate the possibility of a dangerous complication. Sinus lifting is carried out with a good purpose, for example, to build up bone tissue near the bottom of the maxillary sinus so that it is not perforated during implant placement.
In general, bone grafting is almost always tolerated favorably, often it is performed simultaneously with the installation of an implant. But sometimes there are quite harmless side-effects of the time, disguised as complications that can frighten.

For instance:
- Temperature increase up to 37.5 degrees;
- A feeling of heaviness in the maxillary sinus;
- Swelling of the face;
- Small hematomas.
The fact is that the tissues of the maxillofacial region have abundant blood supply (especially the lower jaw), and almost any surgical intervention can be accompanied by phenomena that sometimes even inform informed patients.However, the frightening appearance of edema and hematomas in 90-95% of cases does not correspond to their real danger - that is, it all looks scary, but it is not dangerous to health and does not lead to serious complications.

A decrease in the severity of such edema and hematomas is observed already in the first days after implantation of the teeth (and sinus lift), and finally they usually disappear after 1-2 weeks.
In general, any surgical methods of dental implantation, as well as the stages of bone grafting, can not do without side effects, although in most cases it is not reasonable to consider them complications.
How to distinguish harmless symptoms that occur after dental implants from developing a dangerous complication? Here are a few examples:
- Pain. As already noted above, this is a normal reaction of the body to traumatic intervention, as a rule, easily removed with painkillers. They are prescribed by the doctor after implantation of the teeth or sinus lift. But if severe pain accompanies healing more than 3 days from the moment of implantation, then a complication can be suspected.
- Edema is also a common result of the inflammatory process, occurs 2-3 hours after the intervention. During the week, swelling of the maxillofacial region on their own pass. In case of their preservation after 7 days from the moment of implantation of teeth and, especially, with an increase in size, it is necessary to immediately consult a doctor.

- Bleeding. Intensive bleeding within 8-10 hours after dental implantation most often indicates clotting disorders or problems in the cardiovascular system. If these basic reasons are excluded, then almost always the blood stops safely. The exceptions are injuries of large vessels made during implantation, but such complications are extremely rare and are manifested by severe bleeding, starting from the first day of surgery and more than 5-7 days with the formation of large hematomas.
- Temperature rise. As well as after the sinus lift operation, an increase in body temperature even up to 37.5 within 2-3 days is normal. In rare cases, the temperature on the day of implant placement can rise to high values (above 38.5), especially after implantation of more than 6-8 dental implants, but this is not the result of complications or errors made during the operation, and in 90% of cases it is individual body reaction. A serious complication can be suspected if the temperature not only does not decrease within 3-4 days, but is also prone to some increase, and purulent discharge appears in the places of implant placement (pus may have an unpleasant odor).
- Loss of sensitivity in the face. Loss of sensitivity in part of the face is a rather unpleasant, but not very often observed complication after dental implantation. Usually, decreased sensitivity lasts no more than 3-5 days. If during the implantation the dentist-surgeon suffered serious damage to the nerve, then its self-restoration sometimes ends only within 4-6 months. Recovery can be accelerated by physiotherapeutic methods of treatment and drug therapy, without surgical intervention.
Sometimes the appearance of an unpleasant putrefactive odor in the area of a recently installed tooth implant leads patients to think that a serious problem has arisen - it may be rejection, because “something is rotting and decomposing there ...”
In this case, it is useful to know a number of quite characteristic signs that really warn about the beginning of implant rejection:
- Severe bleeding for more than 3-4 days;
- An increase in edema and its preservation for more than 2-3 weeks;
- Gradual intensification of pain within 2-3 days from the moment of dental implantation;
- Sensation of “moving” a foreign body in the mouth where the implants were placed.
But as for the appearance of bad breath - everything is not so simple here.Such a smell can be caused both by the formation of pus (which may indicate a serious complication), and by the completely natural bacterial degradation of organics, sometimes even under the plug of an implant.
How to prevent negative consequences after implantation?
We note a number of simple rules, following which you can not only significantly reduce the risk of complications after dental implants, but also in some cases accelerate the process of implant engraftment, making it as comfortable as possible.

These are the rules:
- Timely and correctly take the drugs recommended by your doctor (antibiotics, antihistamines, painkillers, etc.);
- Responsibly approach mouthwashes with antiseptics;
- Visually and by sensations, monitor the condition of the installed implants and look after them after implantation according to the scheme prescribed by the doctor;
- Do not smoke at least 1-2 weeks after surgery (in some cases it is required to completely abandon this bad habit);

- Limit chewing on the implant side (as indicated).
It should be borne in mind that only a dentist can choose for you an adequate course of taking drugs, based on your individual characteristics and concomitant diseases. Therefore, the independent choice of one or another home treatment method and drug may be fraught with undesirable consequences (for example, some comrades strive to spread gums with some ointments: Metrogil Denta, dental adhesive paste Solcoseryl or others, although this is not always desirable).
It's important to know
Until the seams are removed, the ideal food is boiled vegetables, light warm soups and fish dishes (boneless). But solid, sticky, floury, and especially sharp and hot dishes can contribute to the development of inflammation in the implant area.
After installing crowns and bridges on implants, it is important to carefully and regularly care for them. Twice a day, you need to brush your teeth and once - interdental spaces. Where the implant is in contact with the gum, it is recommended to clean it from plaque and food debris in the evening with a soft brush for interdental spaces.

Well, of course, the right choice of a dental clinic helps to avoid complications, taking into account the reviews of patients who have already visited it. In addition to the clinic itself, no less, and even more attention should be paid to the choice of a specific doctor who will perform the work, because the final result directly depends on his qualifications.
What implant systems are characterized by a minimal risk of complications
Currently, there are more than 300 types of dental implants, which differ from each other in many ways. However, among all this diversity there are no such implants that would be characterized by zero risk of developing possible complications after their installation.

Meanwhile, there are several really well-proven systems that are rarely rejected with the correct and professionally implemented implantation technology (and the relevant statistics confirm this well).
You can choose the safest implant system taking into account 5 main selection criteria:
- It is highly desirable that the titanium of which the implant is made has a high degree of purification;
- It is desirable that on the surface of the implant there should be both macro- and micro-threads;
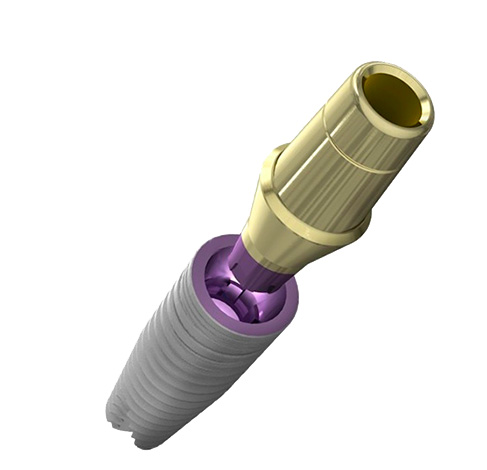
- The presence of a conical connection of the abutment and implant. The conical connection ("Morse cone") is currently one of the most reliable types of articulation and can extend the life of the implant;

- Long-term manufacturer's warranty on the implant system. Some manufacturers give a lifetime guarantee on their products, which indicates the quality of materials tested over the years and the minimum risk of complications when working with similar products;
- The life of the brand in the market. The longer the implant system exists in the dental market, the higher the chance of getting a really high-quality product.
At the moment, dental implants from Sweden, Switzerland and Israel have proven themselves to be the best on all these 5 criteria. At the same time, more and more cheap analogues of Asian origin from companies that have neither a long history nor sufficient experience in using their products have recently appeared. For the low price of dental implants using such analogues, there may be greater risks of complications, for which some clinics are far from always ready to bear responsibility.
Therefore, in order not to become the hero of the famous proverb “Avaricious pays twice”, you should be as responsible as possible in choosing a clinic, doctor, implant manufacturer company and going through the rehabilitation period after surgery. Then the result of dental implantation will be a really high-quality treatment without any unpleasant complications.
Be healthy!
An interesting video about the possible complications that sometimes arise after dental implants
Implantation or classical prosthetics - what to choose after all? ..




Hello! I lost taste after the operation. Ultrasound and other studies have shown that everything is normal. Could this be after dental implants? If so, how to treat?
Hello! Loss of taste in you is unlikely to be associated with nerve damage during surgery (implantation), since the nerves that are responsible for the taste sensations do not pass near the areas where the implants are placed. In extreme cases, sometimes there is a loss of sensitivity in certain areas of the face (including due to edema), but all this cannot be the reason for the loss of taste.
In rare cases, loss of taste after a dental intervention is observed due to exposure to the lingual nerve during anesthesia. Over time, this goes away.
Be that as it may, it is important to accurately diagnose, and only after that take action. To begin with, I recommend seeking advice from a neurologist.
Oh god! Doctors are also suspicious! “The patient thinks that the doctor has disintegrated his entire jaw, and he could have cut it more accurately!” I, as a patient, would think the following: an office was prepared for me, at least two people gathered to conduct the operation, and I chandled something, got scared, let me down. Blood is flowing, they cannot continue ...
Hello, I recently installed implants, crowns have already been installed on them. I want to know if I need to look after them somehow in a special way, or how about ordinary teeth? What care products are better to use?
Hello, Alina. Of course, the issue of hygiene is very important, since any orthopedic structures require even more thorough care than their own teeth. It is necessary to brush your teeth 2 times a day, using, for example, Paradontax toothpaste. 2 weeks after the installation of the crowns, an irrigator can be used.
Hello. Two implants were installed on the lower jaw on the left 6 days ago. I went to the clinic according to reviews. Until now, the 6th day there is pain, forced to take painkillers (3-4 times a day), and the pain comes from a tooth adjacent to the implant - 4 left on the lower jaw. I went to the surgeon who performed the installation. I was about to remove one of the implants, announced that a nerve could be transmitted by this implant. But the doctor himself during the consultation doubted whether to remove the implant or not. Let go home, said to watch a couple of days, the pain will disappear or not.
What do i do? What diagnostics are there to understand if the nerve is affected by the implant or not? At this point in time (6th day), the swelling of the cheeks on the left almost disappeared, there was no numbness of the lips. But there is an almost constant aching pain in the region of the 4th tooth on the lower jaw on the left. Implants are instead of the 5th and 6th teeth on the lower jaw on the left, next to the 4th, which painfully hurts.
I am in an uncertain state and situation.
Hello Renata. In such a situation, it is advisable to conduct an additional study - computed tomography (CT) scan, in order to understand whether the area around the implants hurts or a adjacent tooth.
Implants in the area of 5s and 6s are really close to the chin nerve and, possibly, it was transmitted during installation. There may also be a problem in the 4-ke itself. If the reason is 4-ke, then tooth treatment is required. If the problem is in the implant, then it can be removed, wait a month, wait until the inflammation is removed and then reinstall.
Hello, I was delivered three metal crowns on implants on January 29: on the left 5 and 6, on the right 6. The implants were installed three months ago, everything was fine, no problem. It seemed to me that the crowns - this is nonsense, but it turned out the opposite. Already when I arrived at installing the abutment and taking casts, there was severe pain on the left when screwing the abutment, I even twitched. The doctor said that it was gum, but it seemed to me that the pain was inside, deeper. In the evening I even drank ketans.
In the morning everything was fine, the pain went away, but a week later, when I arrived at the installation of crowns, the pain appeared in the same way. I asked the doctor why it hurts so much? He again said that it was a gum, that before the evening everything would pass! But today is already 01/31, i.e. two days have passed, and everything is aching and aching, and it hurts 4, my next tooth, and not the crown. I can’t chew on this side, it hurts. And on the right, although there wasn’t such, after installing the crowns, there was also great discomfort: when I chew, the jaw from the bottom starts to whine a little. And the crowns do not interfere in height (the doctor did a bite correction), but in width. It seems that I am like a hamster, that I have something behind my cheeks! Tell me what to do? Maybe you need to take pictures? (For some reason, in the clinic, before putting crowns, they didn’t, or maybe it was necessary?)
Hello, Natalia! After analyzing your situation, I came to the conclusion that you need to have a CT scan and consult your implantologist with a picture, telling him about the situation and what worries him. The causes of pain can be several:
1. During orthopedic manipulations, excessive force was applied, as a result of which the implant was turned. In the future, this situation can lead to pain during chewing.
2. The anatomical shape of the crowns is larger than necessary, that is, at some stage of their manufacture, a technical error was made.
3. It is also possible that the crown raises the gum, and correction of the gums and crowns is required.
But I have an ambiguous situation, I don’t know what to do ... After implantation, the cheek swelled the next day, the mucous membrane swelled (well, everything is as it should). There is no pain as such, no bleeding and no odors.Chewing tooth on the lower jaw - a huge opening. This is the point: the bone was thin, a titanium mesh and the implant itself were inserted. As I understand it, a hole for an implant is hammered with sawn bone chips. The next day, everything was swollen around. On the second day, everything is the same. But nearby, somewhere from the section of the incision (2-3 mm from the implant), discharge with bone chips began. Well, I sucked this thing a little ... Squeezed out a little bit. On the 3rd day, tissue swelling decreased almost to normal.
What was it with bone chips? And is this a complication? ..
Alexander! Most likely, the following happened: edema after such manipulations is formed within 3 days. As a rule, the day after a manipulation similar to yours is performed by a surgeon, on which he squeezes the sacred contents so that the edges of the wound do not part and the bone material does not come out. In your case, the edges of the wound parted, and part of the bone material independently came out. To correct the situation and further proper treatment, you need to contact your doctor as soon as possible and tell him everything.
There was no need to "suck out" the bone material, since at the same time you could violate its required volume, and as a result, now the risks of complications in the process of osseointegration are very high.
Good afternoon. I just have a cry from the heart, I really need help ... I have 6 implants installed. Everything went well, nothing bothered. But now, probably a month and a half, one implant became incredibly painful for me, it is located on the top left, it was placed right after the tooth was removed. The doctor took an x-ray and said that everything is fine, take root well, says that it happens ...
BUT ONE hurts, and not all, and it hurts every time more and more, I'm sitting on painkillers. Here, I'm going to go to the clinic again. The clinic is far from cheap, not just “private” ...
Tell me, please, for what reasons can such pain occur? Maybe something in the bone? I have no puffiness and nothing that would alert the doctor. What should I do?! ((
Hello! Pain in the implant area, especially if it occurs only about a month after installation, is a characteristic sign of inflammation. In this situation, the chances of a successful implant engraftment are practically absent. Since your doctor does not notice the problem, I recommend that you seek additional advice from another specialist to get an independent opinion and find out the causes of pain. For now, I only note that with a high degree of probability it may be necessary to remove the implant, followed by reinstallation after 8-10 weeks.
Good afternoon! On 3-4 days after implant placement on the maxilla, there was a strong trigeminal neuralgia from the installation side. Edema, pain and temperature are absent. Neuralgia does not go away, I take B vitamins and diclofenac, although the intensity has slightly decreased. Is this a complication of implantation, and what else can be done?
Hello, Elena. This is a fairly serious diagnosis! In this situation, I do not recommend looking for solutions to your problem on the Internet. You need to contact an experienced specialist as soon as possible to identify the true causes of the pathology (and they can be very different, including those not related to the implantation). Only by identifying the causes of the problem, you can further prescribe the correct treatment, which does not harm your health.
Elena, tell me, did you manage to find out the reason? I have a 1 in 1 situation ...
Two months ago, they installed 2 implants on my lower jaw, everything went smoothly.Now, when pressing on one of them, discomfort appears, which gradually decreases with chewing. No tumors, no redness. Is this a sign of rejection, or is there a hope that he will take root? C-TECH brand implants.
Hello, Elena. Chewing discomfort on the implant is not a good sign. This is not a 100% rejection, but you should definitely contact your implant surgeon and make diagnostic pictures. If a crown is already installed on the implant, then an examination and an orthopedist are needed.
Hello, Doctor! A month after implantation, a bone fragment came out through the gum. What is it? Thanks!
Hello. Perhaps, the surgical protocol for the installation of a dental implant was not followed, and as a result, most problems arise. Please describe the situation in more detail - which tooth implantation was performed for you? Has bone grafting been performed? Sometimes after grafting bone material, its grains exit through the tissue that has not yet healed. Unfortunately, it’s rather difficult to say something specific according to your description. I recommend that you consult a doctor where you will receive the necessary diagnostic pictures and evaluate the situation in the oral cavity.
Hello, Doctor! I have the following case. Two years ago, she installed an implant instead of the last lower (7) tooth and cermet crowns on the top and bottom, a total of 11 pieces. A year and a half later, an infection appeared in my mouth, similar to stomatitis, which, after tormenting me with a low temperature, disappeared, then appeared again, after about a month. And so for a year (treated at home with herbs).
Then the gums began to swell - from the far left upper side. After home anti-inflammatory procedures with herbs, everything went away after about a week. Then the same thing appeared, but on the lower side of the extreme teeth (there are no teeth there, only bridges, and the latter are alive above and below).
Somewhere in a year - the same situation, but already on the lower right side, where instead of a 7-ki is an implant. The edema lasted 14 days - until it started taking antibiotics. No pain in edema. After the medications, the external swelling of the cheeks passed, but not completely on the internal gum. The image shows some kind of infection near the implant. The doctor ordered a CT scan (3D) and said that it was due to false teeth and an implant, and that you might have to remove everything. I'm in a panic. Indeed, the installation of the implant and crowns was easy and without relapse 1.5-2 years ago. Both the experienced doctor and the installation procedure went without any problems.
What do you think it might look like? Is all this a consequence of infectious stomatitis, which I have a suspicion of (I had never had it before, even in childhood, although I have been suffering from gum disease since I was young, periodically treating it). Thanks.
Hello, Tatyana. Without additional data, and based only on your description, we can only assume why these inflammatory processes arose. In general, we can say for sure that the implant normally serves much more than 2 years (even the most budgetary implant today should serve at least 5 years). Accordingly, we can conclude that there is a mucosal disease - this can be either a systemic disease of the oral cavity or a local lesion, usually resulting from the use of teeth as a support for some or other artificial structures (soft tissue is damaged under adjacent construction). In a human case, in order to understand the problem in detail, an examination by a dentist is necessary, therefore I recommend that you consult a doctor as soon as possible.
They put two implants on the lower jaw, after 10 hours the seams parted.The doctor did not begin to impose them again, but said that without seams everything would grow over. How dangerous is this?
Hello Anastasia! The divergence of the sutures is a rather serious situation, because the risk of exposure of the installed implant increases. The final decision on suturing is made by your doctor, but although he believes that there is no need to re-suture, I would still recommend that you re-examine after a short period of time to see if everything really goes as your doctor.
What pills and food are contraindicated in the presence of a tooth implant?
Hello, Altynay. In the presence of implants in the oral cavity, the use of hard foods such as nuts, chocolate roasted potatoes, raw carrots, etc. is not recommended. This is due to the fact that implants, unlike natural teeth, are more vulnerable to critical mechanical stresses. As for drugs - there are no definite contraindications. All appointments are usually made based on the individual tolerance of a particular drug, the focus of treatment, and should be agreed with the attending physician.
Hello, Doctor! Three implants were installed at the bottom right: 4, 6 and 8. To describe the further for a very long time, the mandibular canal, hematoma, its decomposition, my struggle for salvation, four-month rinsing of the decomposed hematoma, fistulas with a hypertonic solution were affected. In general, I raked in full, I thought that I would die. The result - osteomyelitis, was operated on, the bone was cleaned, and the implants were removed. I have a mechanical aortic valve, the implantologist knew. What to do next, completely at a loss. If you repeat the implantation, the clinic said that no earlier than a year later, with bone growth. Maybe you already forget about the implants and put a removable denture, because after a year the bone on the right, without having a chewing load, can begin to collapse? After what time can I put a removable denture and is it necessary to build a bone? After all, a large depression has formed.
Hello Vera! If re-implantation is supposed, then in this situation it is really necessary to wait for the complete healing of bone tissue and restoration of the mucous membrane. It will take from 6 to 12 months. After that, you will need to do a CT scan again. Is it worth it to reinstall the implants - it's up to you, but I’ll note that if everything is done correctly, the risks are minimal. You can also consult an implant surgeon about implantation with immediate loading.
If you still refuse re-implantation, then the option of manufacturing a removable prosthesis will be a normal alternative. The advantage of this method of prosthetics is that you do not need to build bone tissue. After 6 weeks after the last surgical intervention, it is already possible to start manufacturing a removable prosthesis. One should only bear in mind that a removable prosthesis will be less comfortable to wear than with prosthetics on implants.
Hello! At the end of August, 4 implants were placed on the upper jaw with bone grafting. It seems that everything heals normally. But one moment annoys me. In different parts of the bones of the face and head, there is a feeling of pressure. As if the skull is squeezing. Or is it paranoia?
Hello Arina. The symptoms you described may not be related to implants. Usually, if any problems arise, then pain or other discomfort is localized in the area of the problem implant. If everything heals normally, there is no inflammation and pain - it makes sense to also look for a pathology that is not related to the implantation.Therefore, I recommend making an appointment with two doctors: an implantologist and a general practitioner.
Hello! Is it normal that bone atrophy occurs even after implant placement? 7 months after installation, I notice that the bone tissue on the sides of the tooth has narrowings (depressions) on the external and internal sides of the jaw.
Hello Roman. Bone tissue atrophy after implant placement is possible for a variety of reasons (general causes, medical error, inflammatory phenomena, etc.). To one degree or another, atrophy of bone tissue occurs for many types of implants, but usually it stretches for many years.
So, according to only one brief description of the problem, an exact answer to the question will not work. To consider your particular case, it is necessary to conduct a study, to do a computed tomography. Therefore, I recommend not waiting for the situation to worsen - it is better to turn to an implantologist surgeon for a consultation now.
Hello, Doctor! A year ago, there was basal implantation on the upper and lower jaws. After the installation of permanent prostheses, the lower jaw began to move forward during the conversation, there were also problems with diction: sounds Ж, Ш, Щ, З, С and sometimes R. What are the reasons? With temporary prostheses, everything was fine. Thanks!
Hello Maria! Judging by the description of the problem, I can assume that with constant prosthetics, the setting of artificial teeth was changed (that is, they began to be different from what they were in the temporary prosthesis). If the problem persists, in such cases, you should contact your doctor (orthopedic dentist) for correction.
In mid-November 2018, they underwent an implantation, after which I almost gave my soul to God - so much pain, temperature up to 38, suffered a double abscess. They removed 2 implants, and what will happen in the future - I do not know, I'm afraid for further rejection. What should I do? I followed the doctor’s recommendations correctly, but I suffered pain ...
Hello, Tatyana! As with any other operation, there is always a risk of complications with dental implantation. And most likely, your clinical situation was just connected with a postoperative infectious complication (peri-implantitis). The consequence of this was an increase in temperature, pain, the development of an abscess - in such cases, removal of implants is really required.
Fortunately, all this does not exclude the possibility of re-implantation, in preparation for which increased attention is paid to preoperative hygiene and antibiotic therapy - this minimizes the risk of infection of a surgical wound.
I advise everyone to implant. The most important thing is not to be afraid, choose a good clinic and solve problems, especially when it comes to standard prosthetics.
Hello! I have 2 implants in my lower jaw that hurt, and the doctor refused to remove them ... For 3 months I could not install crowns on them, after very painful manipulations. The crowns came tall and wide, not in size, but he still screwed them with a big pressure, after which my gums swelled up and hurt for 2 days. On the 3rd day I came to him, he unscrewed the crowns and gave them to the laboratory to cut them from below, while with irritation he declared that my gums were to blame for not accepting them ...
After turning from the bottom, I installed it, but then the problems started: the crowns shifted to the sides and grew into the gums. The doctor twisted them with great difficulty and with painkillers, then smeared them with Selcoseryl and again set them temporarily. At the same time, one tooth was bleeding, and pus came from another ... After my questions and after 15 such manipulations, the doctor returned the money for the crowns and sent me away, saying that everything was fine with the implants, and I would put the crowns with other doctors.
But the implants are inflamed, and I turned to my doctor for removal, but he refused. I asked for a copy of the treatment from the medical record, but the doctor said that it was a medical secret, and did not give it out. But at my request, I wrote a certificate that refuses to delete.How to be The question, as I understand it, is that he avoids paying money for implants. Before opening the gums, the implants were not sick.
Hello, Olesya. For a more accurate determination of the condition of the implants, sign up to another doctor, ask for an OPTG, CT scan and an aim shot. In the presence of an inflammatory process, especially purulent, implants are usually removed. You probably have a contract with the clinic, which should be written warranty, so that just "back home" you can not send.
They placed 4 implants on the upper jaw, removing first 4 teeth on the left. After this operation, there was swelling, fever up to 38 degrees and so on. And then there was very severe dizziness and shortness of breath, darkening in the eyes and severe weakness. This has been going on for a month and a half. I accept Betaserk. Could such a condition be the result of a cerebrovascular accident?
Hello, Galina! It is possible that the symptoms you indicated may be caused by a feature of cerebral circulation, however, the operation to install dental implants can in no way affect cerebral circulation. In this situation, I would recommend contacting a general practitioner.
I’m also thinking about whether or not to put an implant (the tooth broke off at the level of the gums). Everything is so complicated.
After implantation, after 2 hours, a blood clot formed near the implant. Please tell me, is this the norm?
Hello, Tatyana. The description "near the implant" is not entirely clear. If you mean the gingival mucosa, then this is the norm. However, in order to dispel all doubts, it makes sense to sign up for an examination with a specialist who installed the implant.
Hello, two implants were installed on my lower jaw instead of 6 and 7 teeth. Immediately after the operation, there was swelling. After 5 days, lincomycin was prescribed for a week. They also opened the lymph node, there was blood in it. All this time, the temperature keeps no higher than 37. Almost a month has passed, now there is no swelling, no temperature, but aching pain is constantly present, especially at night. I have to take painkillers. Another gum is slightly inflamed. The doctor said that I have such a feature of the body, said to wait and everything will pass. I am 45, I followed all the recommendations of the doctor. Tell me, is everything going well and why can it hurt for so long?
Hello, normally puffiness can persist from 3 to 5 days, in the next 7-10 days the pain should stop. Judging by your description, there is inflammation, and it is highly likely that this is peri-implantitis. Therefore, I recommend contacting your doctor (or another doctor in order to obtain an independent opinion) for examination and further actions.
Hello, after installing the implants, instead of 6 and 7 from the bottom left, numbness went away after three months (on the chin, lower lip, gum on the left), but neuropathic pains do not go away. Everything lasts 9 months. An X-ray showed that 7 stands just 1.4 mm from the mandibular canal, the implant is surrounded by bone tissue, and there is no inflammation. What to do, remove the implant or not? After all, it can still affect the nerve if it was damaged.
The doctor does not recognize the damage to the canal. Electromyography of the motor part of the nerve showed mild axonopathy. Can an implant irritate a nerve? The neurologist says that carbamazepine will not help if there is a problem in the hole, I started drinking it after seven months, before that I was treated on the peripheral system. I don’t know what to do - to remove or not the implant that has taken root.I really look forward to your consultation.
Hello! If the bottom of the implant is located more than 1 mm from the mandibular canal, then it is not recommended to remove the implant in such cases. In addition, as follows from your description, there is a positive trend. Sensitivity restoration 3 months after surgery is a good sign that allows you to count on a positive prognosis. I would recommend that you conduct an observation in dynamics for another 3 months. After that, sign up to the doctor and make a decision on further actions.
Can a chewing tooth implant be done with bruxism?
Hello Anna! With bruxism, you can do an implantation on the chewing group of teeth. It is usually necessary to undergo training before prosthetics in the form of Botox injections into the masticatory muscles (according to indications), or a high-quality grinding of the crown on the implant and the use of a special night mouth guard are necessary.
Hello. After installing the implant, I got a strong tumor, very strong salivation began. Now I can’t sleep. What to do?
Hello, Tatyana. First of all, follow all the doctor's recommendations (including regarding the intake of tablets that you should have been prescribed). In the absence of positive dynamics, be sure to consult your doctor.
Good afternoon! After 2 months of implantation "all for 4" there was a feeling of pressure on the sinuses. Mucous transparent discharge from the nose also appeared. This is normal?
Hello, Natalia. You describe the symptoms associated with a typical disease - sinusitis, but also, this may be the result of an operation to implant a tooth. You need to contact the doctor who performed the operation for an examination and diagnosis, after which a decision will be made on the need to refer you to an ENT doctor or additional treatment through dentistry.
They put 2 implants on the lower jaw. Five months later, they began to try on crowns, I felt pain. Now the gums are swollen and sore. The doctor said that everything is fine with implants. But why did the gums hurt? Already 3 days it hurts.
Hello Denis. It is possible that when trying on the crown, the gums were simply infringed, as a result of which it was swollen. However, if the inflammation does not go away after a few days, then you may need to do an x-ray to assess the condition of the bone tissue around the implant. In the event that for some reason the implant did not integrate with the bone tissue, it will not be stable and will have to be removed (but judging by your description, this is an unlikely option).
Hello. She installed the implant, put a crown on it. But the crown does not adjoin to teeth, cracks remain and food is constantly clogged there. Is this normal?
Hello Irina. Definitely, this is not normal. The crown should fit snugly, and constant jamming of food is unacceptable, as this can lead to inflammatory processes. You need to contact your doctor to eliminate these shortcomings in treatment.
I had a bone grafting operation with an autobone fence. There was severe swelling, which fell slightly on the 3rd day. Today (about a week later) the edema stands still. In addition, as the doctor said, a large hematoma formed near the gum.I keep drinking antibiotics. Tell me, is swelling and hematoma dangerous? Can all this resolve itself? The cheek turned yellow, a bruise on the chin. There is no temperature, but the hematoma does not decrease.
Three weeks passed after the installation of the implant with simultaneous bone grafting. After 1.5-2 weeks, the gums periodically swelled and the pain gave into neighboring teeth. Now there is no pain, but on one side of the implant there remains a blood clot. Is this normal at this time?