Next you will learn:
- Is dental implantation performed during periodontitis today, and what difficulties can be observed?
- What exactly happens in the oral cavity during periodontitis and periodontal disease and how these processes affect the success of the implantation procedure;
- What are the options for prosthetics, depending on different clinical situations;
- What types of implants can be used if the patient has periodontitis (periodontal disease);
- What is important to pay attention after dental implantation is already at home, to prevent periodontitis from continuing its destructive work.
Periodontitis today is almost as common a disease as tooth decay, and often leads to mobility and multiple tooth extraction. The question of whether it is possible to put implants in periodontitis has ripened from the very moment when the technology of dental implants has just received its scientific justification and gradually began to gain popularity. Doubts of doctors about the feasibility of implantation arose with respect to a disease such as periodontal disease (which occurs in approximately 1-3% of patients).


Generally speaking, dentists were divided into two camps: some believe that implantation of teeth with periodontitis and periodontal disease is a very dubious event. However, others, on the contrary, note the high efficiency of prosthetics on implants even in the presence of these diseases.
Moreover, the approach to the problem itself is of particular interest. For example, maxillofacial surgeons and implantologists consider it a waste of time and money to “strengthen” bad teeth on the background of periodontitis and, moreover, periodontosis, while periodontologists introduce the latest developments related to the preservation of teeth from extraction against the background of these diseases and strongly advocate that such teeth need to still try to save.
On a note
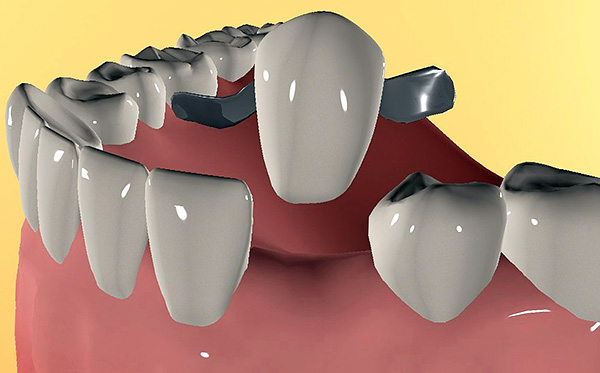
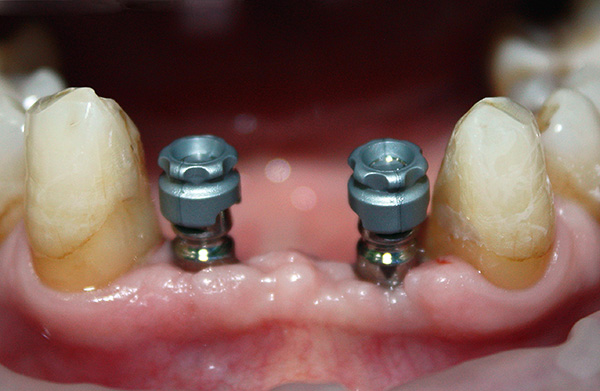
Dental implantation is an innovative method of prosthetics, which allows you to replace lost or problem teeth by implanting metal “roots” in the jaw, followed by fixing crowns on them. Such crowns on implants allow not only to imitate natural teeth in an aesthetic plan, but also to return the lost function (chewing) with the restoration of a full bite.

So is it possible to place implants for periodontal disease and periodontitis, and in which cases, to prefer this approach? In order to better understand the specifics of the problems and difficulties that may arise in this, let's first look at what exactly happens during periodontitis and periodontal disease with the tissues surrounding the tooth ...
What happens in the mouth with periodontitis and periodontal disease
The precursor to periodontitis is most often gingivitis - inflammation of the gums that occurs without compromising the integrity of the gingival joint. Gingivitis can appear in childhood and adolescence due to the accumulation of bacterial plaque on the teeth due to improper orthodontic treatment, stress, smoking, immune disorders, acute and chronic diseases, malnutrition, malocclusion, insufficient oral hygiene, lack of adequate dental treatment, etc. .d. Bacteria (less often fungi and viruses) become the direct cause of the onset of inflammatory processes in the gums, which sooner or later turn into periodontitis.

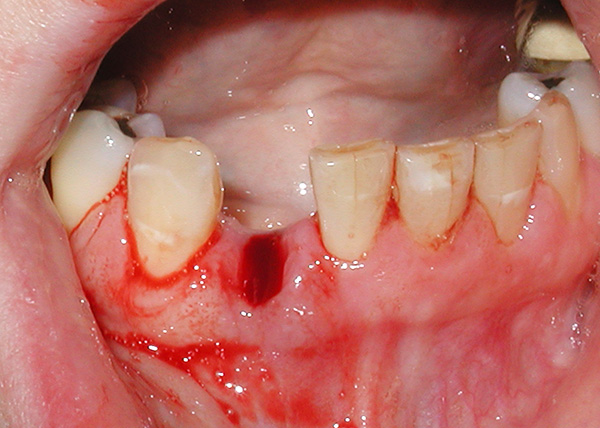
Periodontitis is one of the most common causes of tooth loss, since as a result of the progression of the disease, the dental "cells" in which the tooth is held are literally destroyed.At the initial stages, the symptoms of periodontitis are insignificant: against the background of abundant dental deposits (stone, plaque), bleeding of the gums occurs, sometimes even a slight tooth mobility can be observed.
But exacerbations of the disease are extremely difficult from the point of view of the person’s symptoms and psychological state: in addition to severe bleeding from the gums, suppuration starts from the tooth pockets, strong tooth mobility with displacements, pain and burning in the gums, bad breath and active loss of the jaw bone . All this in aggregate, in fact, can create certain problems for dental implantation.

Unlike periodontitis, periodontal disease is not an inflammatory disease. Therefore, with periodontal disease there are no gingival pockets, suppuration and tooth mobility, but against the background of their good fixation, the neck of the teeth is exposed with progressive bone loss. Reducing the height of the interdental septa against the background of foci of osteoporosis often leads to tooth extraction, and since periodontal disease is not a local, but a generalized disease, almost all teeth that have lost bone support are removed.
It is interesting
A number of dentists (mainly maxillofacial surgeons) believe that such a disease as periodontal disease does not exist at all, preferring to isolate only periodontitis, as an extreme form of gum disease, leading to tooth loss. However, supporters of the traditional approach do not want to recognize their views as obsolete and until today in the dental practice they use the working classification of diseases according to ICD-10, where periodontal disease is indicated by code K05.4, and chronic periodontitis is indicated by code K05.3.
So is it possible to place implants for such problems with the gums?
It would seem that dental implantation during periodontitis or periodontal disease amid disturbances in gingival attachment and loosening of teeth can be a real help not only in restoring the dentition, but also in preventing further destruction of the bone (the load on the bone tissue prevents its loss).
Let's look at the most common clinical situations:
- All teeth on the background of periodontitis should be removed;
- A significant portion of teeth during periodontitis can still be preserved;
- The patient has generalized periodontal disease.
Situation 1: all teeth on the background of periodontitis should be removed
In fact, the first situation, despite all its tragedy, is still a fairly common reason for patients to go to the dentist. The fact is that Soviet dentistry at one time formed many people with a strong fear of dentists, and even the approach to the treatment of periodontitis left much to be desired. Therefore, people of 45-60 years with signs of severe periodontitis are still turning to dentists, when it is already impossible to save the remaining moving teeth.

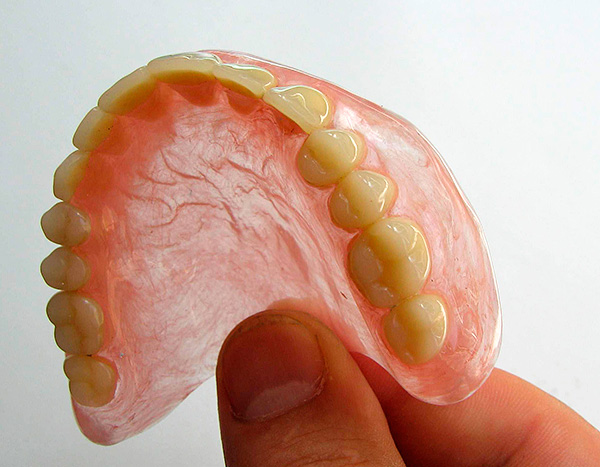
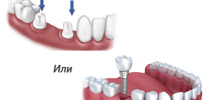
After cleansing the oral cavity of hopeless teeth, a person has only two ways: either to wear removable dentures, or to perform prosthetics on implants.
The option with complete removable dentures, of course, is many times cheaper than dental implants, however, it should be remembered that removable dentures are characterized by certain disadvantages:
- They do not stop atrophy of the bone tissue of the jaw, and in some cases even aggravate this process;
- The second drawback is a long period of getting used to removable dentures;
- In addition, in 60-70% of cases, removable dentures do not satisfy either aesthetic or functional parameters (in other words, they do not color the person much and are not very comfortable to wear and chew).
As a result, today most dentists are inclined to argue that the installation of dental implants for periodontitis is the only correct and promising solution, especially with complete loss of teeth.
Moreover, there is a scientific justification for this approach: own teeth in the mouth connect to the alveolar bone through the ligamentous apparatus of the tooth (periodontal tissue). It is in the ligamentous apparatus that there is an infection leading to progressive loss of bone tissue during periodontitis. After the extraction of all teeth together with the infected ligamentous apparatus, the osseointegration of the implant, that is, its fusion with the jaw bone, will pass fully, and due to chewing load, further bone loss will be prevented.


Situation 2: a significant part of the teeth with periodontitis can still be maintained
Consider the second case, when most of the teeth with periodontitis can still be saved. Everything is not so clear here. The fact is that long before implantation in dentistry there were many developments regarding the strengthening of mobile teeth - for example, splinting them.
The classic version for that time was associated with the technique of "linking" the teeth together by welded crowns. It’s easy to understand this tactic: a group of moving teeth came together, turning into a single whole, which made them more resistant to mechanical stress, and for a long time. Currently, a popular option for splinting teeth is to “bind” them using aramid floss and fiberglass.

Therefore, if all teeth (or almost all) are retained in the oral cavity with the initial form of periodontitis, complex treatment of periodontal tissues can be carried out using modern devices (ultrasound, laser, etc.) and the latest technologies.
On a note
However, it should be remembered that periodontitis, according to modern scientists, is an incurable disease, although it can be converted into a stable remission with the preservation of their teeth for many years. True, for this, especially in advanced cases, it will take a lot of time and money to carry out complex manipulations with the periodontist with constant monitoring (2-4 times a month) and corrections according to the indications of periodontal treatment.
If, for some reason, gum treatment becomes ineffective, then tooth extraction is performed, requiring immediate replacement of the defect. The danger of leaving the resulting “gap” between the teeth is that the teeth left without their neighbors on the background of chronic periodontitis slowly but surely begin to “disperse,” which leads to malocclusion and multiple loss of other teeth in a short time.
Here it is necessary to correctly determine the plan for restoration of the dentition, without delaying for a long time. But what is better to choose taking into account the existing periodontitis: put the usual "bridges" (prostheses), or still spend more expensive prosthetics on implants?
Of course, the doctor selects a strictly individual further plan for a treatment that is appropriate in each case. However, it is worth remembering that in the severe stage of periodontitis, even after a long course of treatment, there remain serious risks of violation of the gingival attachment in the area of those teeth that the dentist can take under the support of the bridge (and there are many such cases).
Each year, 30 to 40% of cases of tooth loss are recorded along with the “bridges” within 1-2 years after prosthetics. That is, there is no absolute guarantee that after the intervention of the periodontist and the course of treatment lasting from 2-3 months to 1-2 years, the destruction of the jaw bone will not continue further. A decrease in bone in the future implies serious problems, ranging from multiple tooth extractions to additional difficulties with prosthetics and implantation.
Therefore, dentists adhere to a reasonable tactic of choice: if there is an initial stage of periodontitis, then they carry out complex antibacterial and anti-inflammatory therapy for reliable teeth,and implants are placed in place of the missing teeth. The main rule here is that there should be no teeth near the installed implants with pathological gingival pockets with pus and infection, otherwise the success of the implantation will be doubtful.
If the doctor is not sure about the prospects of the teeth against the background of severe periodontitis, then all the teeth that are not subject to treatment are removed and implants are replaced.

Feedback
“Recently I decided to install two implants for myself at the top and bottom. About 3 years ago, one tooth was pulled out by a cyst that burst and came out with pus, and the doctors simply screwed up the other tooth. He was treated many times and healed to such an extent that the gum between the teeth began to swell and bleed when brushing and even when biting an apple. At one point, he crunched so badly at me that he burst under the gum. In the end, I also tore him up with tears in my eyes.
When the dentist-surgeon looked at me, she discovered that periodontitis had occurred near my last problem tooth due to the constant ingestion of food in the gap, but not on all teeth. Therefore, my gums were so sore and bleeding, and I constantly regretted them with a paste, like a fool, so as not to scatter the wounds ... ”
Anastasia, Moscow
Case 3: the patient has generalized periodontal disease
The clinical cases when periodontal disease is diagnosed are quite simple with regard to treatment planning. The fact is that periodontal disease is a disease that almost always leads to tooth loss. The moment of exposure of the necks of the teeth with progressive loss of bone tissue of the alveoli is especially difficult for people to tolerate. Therefore, the most suitable treatment tactics for periodontal disease is tooth extraction and implant placement (best of all).

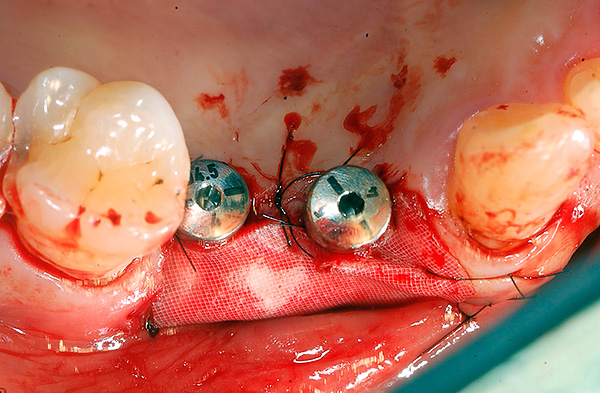
Since there is no inflammatory process during periodontal disease, there is no need to specially prepare the oral cavity for implantation, therefore, most implantologists adhere to the tactics of tooth extraction and implant placement at a time. Thus, it is possible to stop the progressive destruction of bone tissue due to the return of the usual load. Sometimes, in severe cases, it is first necessary to restore the lost bone (sinus lift), and only then - implantation.
Partial and complete removable prosthetics without implantation during periodontal disease does not stop the processes of atrophy of the alveolar processes, and often even exacerbates them.
On a note
The surface of the implant is such that after “splicing” it with the bone tissue, the structure becomes stronger than in the case of a native tooth. With the right choice of the implantation system and compliance with the technology of implantation, even with periodontitis and periodontosis, installed implants can fully serve up to 25 years or more.
An important nuance, taking into account the individual characteristics of the bone tissue of the alveolar processes of the jaw, is the number of implants installed, which should provide the optimal load on the bone tissue to prevent its further atrophy. Durability is determined not only by the qualifications of the implantologist, even with the latest and most advanced techniques, but also by observing the rules of hygiene and caring for the finished structures by the patient himself (see below).
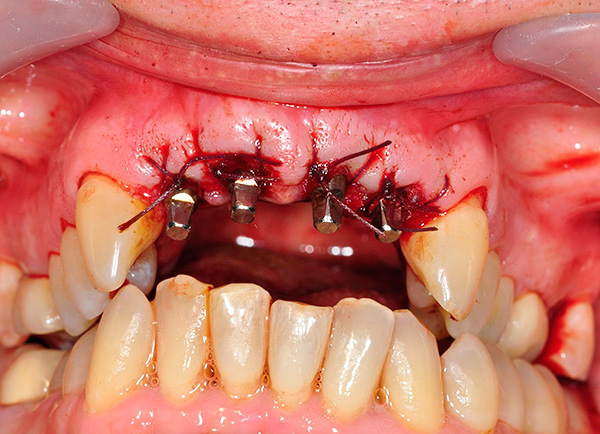
How is implantation performed during periodontitis and periodontal disease
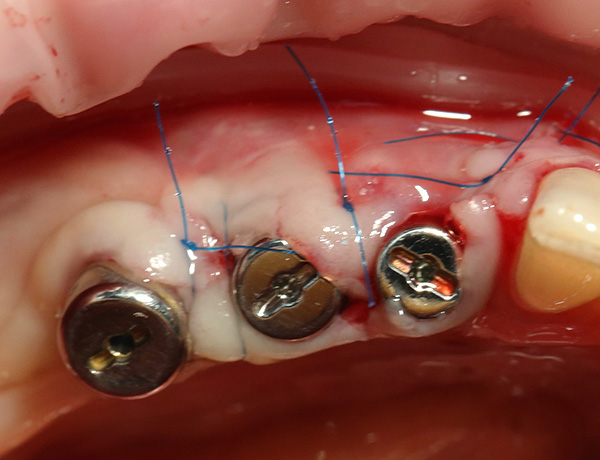
Periodontitis implantation usually takes place in the following several stages:
- Preliminary preparation for implantation;
- The choice of implant system;
- "Implantation" of implants;
- Implant prosthetics.
The preliminary stage is one of the most important, as it helps to minimize risks during and after implantation. It includes a whole program for the treatment of an underlying disease, that is, periodontitis or periodontal disease. Depending on the possibility of preserving the teeth in the oral cavity, an individual treatment plan is drawn up.

For example, if we are talking about preserving tooth groups during periodontitis in the initial stage, then preliminary preparation before installing implants can be carried out according to the following scheme:
- Professional toothbrushing from tartar and plaque;
- Therapeutic (dressings, ointments, etc.), surgical (patchwork, curettage, etc.), orthopedic (selective grinding of teeth, splinting, etc.) and orthodontic treatment of periodontitis;
- Removal of teeth that are not subject to preservation.
Properly conducted treatment of the underlying disease can significantly reduce the risk complications after implantation (eg, rejection of dental implants) In the area of installed implants there should not be sites of an active inflammatory process.
Equally important is the general condition of the oral cavity (level of hygiene, oral care) and the formation of the right habits.
But periodontal disease is not always amenable to conservative treatment, and the process of bone atrophy can occur more intensively every year. That is why the success of further treatment depends on the tactics of the doctor in each case. Most often, preparation for periodontal disease is reduced to the removal of all unsuitable for functional and aesthetic indicators of the teeth, followed by implantation and prosthetics.
Of particular interest is the choice of technique for implantation of implants on the background of periodontitis or periodontal disease. At the moment, implantologists usually choose the following options:
- Classical implantation;
- Express method;
- Basal implantation.
What technologies and implant systems are best suited
Each of the above three implantation technologies is selected for a particular patient, taking into account the severity of periodontitis or periodontal disease. In addition to the degree of bone tissue atrophy, the doctor also takes into account the patient’s age, the presence of concomitant diseases, features of the maxillofacial region, etc. It is an integrated approach at the initial stage (diagnosis) that allows you to choose the right method of implant placement.
Modern clinics, taking into account the above points, most often tend to the express method and basal implantation. The fact is that classical implantation is two-stage and is not performed immediately after tooth extraction. And after implantation of the implants, more than one month passes before the doctor starts prosthetics.
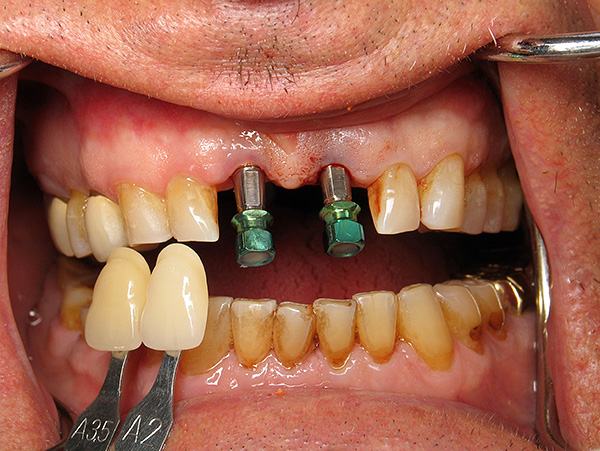
In contrast to classical implantation, the express method even allows for periodontitis or periodontal disease (if indicated) to perform a one-stage implantation immediately after tooth extraction. This speeds up the process of bone regeneration, reduces the level of invasiveness of the intervention and the risks of infection of an open wound. However, for the express method, it is especially important to observe all the technical nuances, which are numerous, and to carry out careful monitoring during the installation of implants.
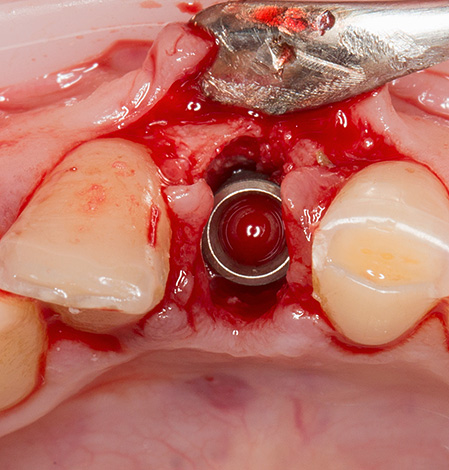
As for basal implantation - it is used for atrophy of bone tissue, which often accompanies periodontitis and periodontal disease. Sometimes only this technique is suitable for significant loss of bone tissue. Such implants are implanted immediately with the abutment (the transitional part on which the prosthesis or crown is fixed) at an angle to where the bone tissue is sufficient for maximum stability.

The structure and shape of basal implants can withstand heavy loads and stop further bone atrophy. After 5-7 days, it is necessary to make prostheses, which should give an immediate load. Such a short period from implantation to prosthetics gives basal implants significant advantages - many patients are very happy to get a beautiful smile just a few days after tooth extraction.
On a note
Classical types of implantation can be carried out even with significant atrophy of the bone, but with a preliminary sinus lift operation: if the bone is not enough to fix the implant or it is too loose, then the dentist first builds bone tissue (sinus lift) in those areas where future implants will be installed. As soon as the recovery period passes, the doctor establishes them and then works according to the standard treatment protocol, up to the final prosthetics after 4-9 months (sometimes 1-1.5 years), depending on the specific clinical case.
The choice of an implantation system is a crucial stage, which should be approached in the most serious way. Today, when choosing a particular implant variety, they are guided by three main criteria: guarantee, stability, cost.

Today there is a kind of implant rating according to these criteria.
So, for example, the following implants belong to the premium class:
- Astra Tech (Astra Tech) - implant system from Sweden. Today it is one of the most popular due to excellent technical characteristics, ease of use and most importantly - a long guarantee and stability of engraftment;
- Nobel Biocare is one of the most expensive designs, which is of high quality. This type of implant is suitable for different clinical situations;
- XIVE (Xive, Germany). Also very high quality implants;
- Anthogyr - the French system.
And some others.
Medium price implants - for example:
- Schutz (Germany) - collapsible and non-collapsible structures;
- Zimmer (USA) - mini implants, standard varieties, as well as implants for implantation into a thin bone;
- Niko - Russian implant systems, which are created from German components.
Some implant systems from Israel (for example, AlphaBio) are heard by many medical practitioners and are in demand among the Russian population due to the relatively low price. In quality in certain clinical situations, they are not inferior to the most expensive implants from Germany and Sweden.
With regard to Chinese, some Russian and Ukrainian implant systems, many dentists are skeptical about the dubious characteristics and average stability, although there are more than one hundred implantologists who successfully install thousands of such structures every year. As they say, how many people - so many opinions.
Features of care for implants at home: how to prevent periodontitis from continuing its destructive work
The success of prosthetics on implants is affected not only by the preparation and stages of implant placement, but also by postoperative home care of the structures. This is especially important with persistent periodontitis or periodontal disease, when the success of implantation directly depends on the implementation of special rules.

Rule number 1.
Dental implants need more thorough hygiene, as the risk of developing periodontitis in their area is significantly higher than in the case of native teeth. It is especially important to treat the back of the implant, where plaque is more likely to form. Poor hygiene creates an additional risk of structural rejection.
Rule number 2.
Contact (interdental) surfaces should be flossed. However, some dentists treat such threads negatively, such as risk factors for permanent gum injury due to inept use, therefore, they are inclined to other methods of clearing gaps, for example, using interdental brushes or irrigators. Moreover, the irrigator allows not only to successfully clean even the most remote and inaccessible areas, where a lot of food remains accumulate, but also improves blood supply to the gums, massaging them.
Rule number 3.
It is important to visit the dentist at least once every 6 months for professional cleaning of teeth and dental implants along with the designs.
It is especially important to follow the doctor's recommendations in the first postoperative stages, when any trifle is important. For example, in almost all clinical cases, the first time after the installation of implants (especially with periodontitis and periodontal disease) you can not smoke, drink alcohol, play sports and hard physical labor. You should adhere to a sparing diet, take the necessary medications and carry out, in addition to cleansing your teeth from plaque, antiseptic rinses of the oral cavity.
All this allows you to significantly increase the life of the implants, up to a lifetime of operation without any problems.
Be healthy!
Interesting video: what to choose, implantation or classical prosthetics?
About the stages and complications of periodontal disease, as well as implantation in this disease



Very informative article, all competently, all the pros and cons. I really liked it.
5 years ago, gums began to bleed. I went to the dentist, he advised me to buy a rinse aid. At the same time, the already exposed tooth root was sealed. Every year I went to the dentistry with one problem - fillings fell out and bleeding gums. Until they came full tryndets. And now they offer implantation, the question price is 300-400 thousand. Moreover, all the villains in white coats are not treated in urban dentistry, but they offer to go to pay, where they themselves earn extra money (burn them in hell with a blue flame).
Well done
I liked the article, everything is painted in detail. I was just worried about the issue of implantation in periodontitis - the doctor offers a bridge, but after reading this article, I learned that the supporting teeth of the bridge can also fall out during periodontitis. Thank you very much for the good article!