
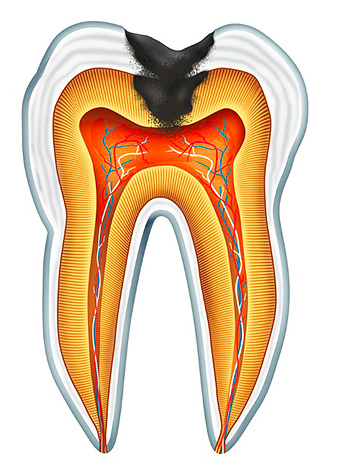
The process of necrotization of pulp tissue (the so-called dental "nerve") in chronic gangrenous pulpitis is preceded by a stage of its inflammation, which is the result of a reaction to the action of certain irritants. Most often, these are bacteria and the toxins produced by them, which enter the pulp through a deep carious cavity in the presence of perforation of its bottom and communication with the pulp chamber, or through a system of dentinal tubes passing in the dentin layer. Sometimes an infection can enter the pulp chamber through a periodontal pocket (from under the gums) or enter the bloodstream for infectious diseases, but such a retrograde infection pathway without caries is extremely rare.
Chronic gangrenous pulpitis is the result of acute diffuse or (less commonly) chronic fibrous pulpitis. In the acute stage of inflammation, the body's immune forces are activated and leukocytes go out to fight the infection in the pulp, as a result of which there is edema (an increase in size) and the formation of fluid: first, serous, and then purulent.
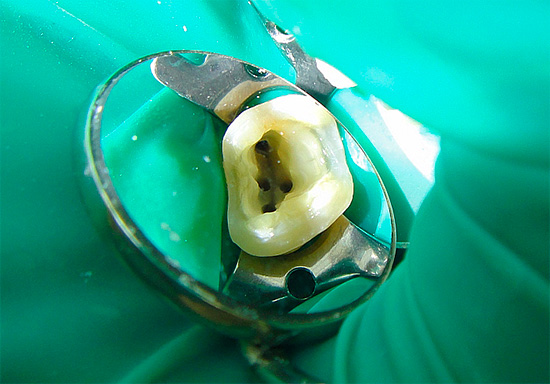
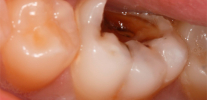
The photo below shows the inflamed pulp removed from the tooth even before it underwent purulent fusion:
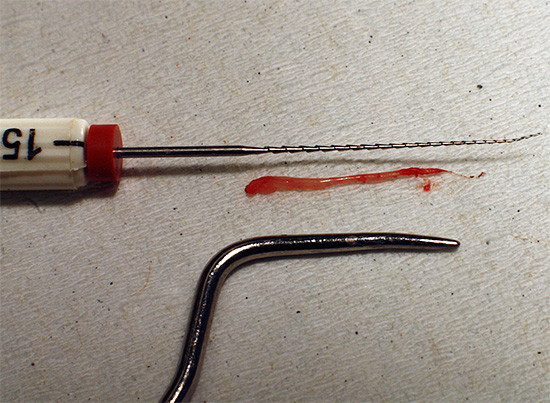
Purulent exudate is nothing but the result of mass death of leukocytes and bacteria. The accumulation of exudate inhibits the metabolism in the pulp, and it begins to die gradually.
So against the background of acute diffuse pulpitis, the “nerve” disintegrates, which precisely determines the most severe bouts of pain, which often pass along the branches of the nerve into the ear, temple, eye or back of the head. As soon as the death of the coronal part of the pulp and the opening of the bottom of the carious cavity with the release of purulent exudate occurs, a noticeable relief occurs - the transition acute form into gangrenous pulpitis.

Chronic fibrous pulpitis passes into the pulp gangrene only through the phase of exacerbation, when new foci of abscess form in the tissues of the “nerve” as a result of disturbance in the outflow of exudate (for example, when the bottom of the carious cavity is clogged with food), which sooner or later turn into chronic gangrenous pulpitis.
Features of gangrenous pulpitis
The ingress of putrefactive microflora into the pulp chamber catastrophically affects the further fate of the pulp. The more active microbes and their toxins, the faster the decay (necrosis) of the “nerve” and the death of the coronal part of the pulp with a gradual transition to the root. The name of the disease directly points to gangrene of soft tissues, which determines the characteristic history of the disease in chronic gangrenous pulpitis.
So, most often complaints of putrefactive breath, aching pains from hot, which persist for a long time even after elimination of the irritant, predominate. There is a feeling of "bursting" inside the tooth, which corresponds to edema of the "nerve" and a slow outflow of exudate from the tooth cavity.
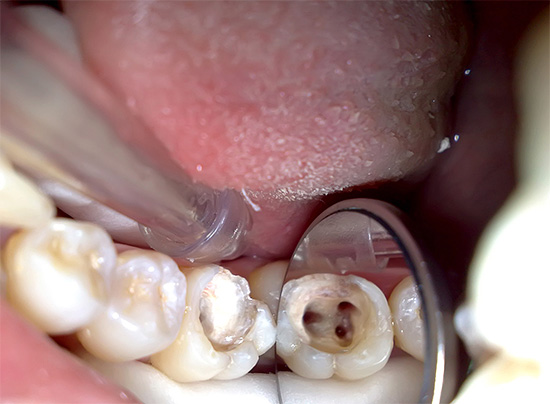
If the message carious cavity with a pulp chamber, where the collapsing "nerve" is located, good and unhindered, then with gangrenous pulpitis there can be no pain symptoms at all. In such cases, the patient indicates only a change in the color of the tooth - the appearance of a grayish tint.
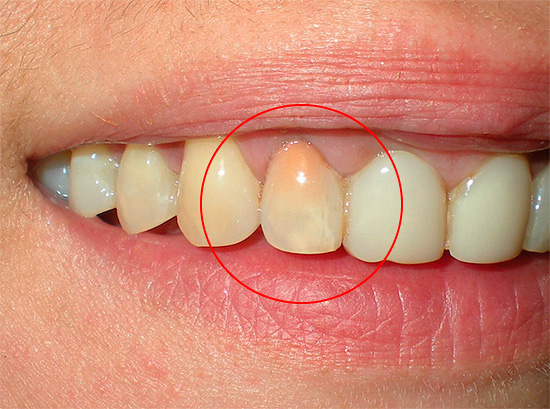
Photo of a tooth with chronic gangrenous pulpitis - an unhealthy gray shade is clearly visible:

In addition to taking into account the characteristic symptoms of chronic gangrenous pulpitis, the dentist also examines the data of objective research methods to make a final diagnosis. For this, a visual examination of the cavity is carried out, palpation of the gums near the tooth, sounding and percussion.As additional methods, thermometry, EDI and radiography can be used.
When examining a tooth, its gray tint is usually striking in the presence of a carious cavity extending deep into the mouth of the root canals. When probing, the presence of a large amount of carious softened dentin is noted, and deep penetration by the sharp end of the probe into the mouth of the root canals is often painful, although pain sometimes occurs when a part of the root pulp is killed.

In chronic gangrenous pulpitis, percussion (tapping on the tooth) is most often painless, but with gangrene of the majority of the pulp and poor outflow of purulent exudate, there may be minor pain. Palpation of the gums in the projection of the apex of the roots of the diseased tooth does not cause pain, since there is no exit of pus through the tops of the roots towards the gums.
For thermometry, the dentist uses a heated tip of the instrument, since it is impossible to diagnose with hot water because of the risk of burns of the mucosa. Typically, the tip of the dental probe is heated above the flame of the burner and carefully brought into contact with the crown of the tooth for a few seconds.
In the presence of chronic gangrenous pulpitis, in this case, a slow increase in pain occurs, which does not go away for a long time - this indicates the presence of purulent exudate against the background of decay of pulp tissue. Almost does not respond to a cold tooth, since most of the "nerve" has already died.

In the framework of differential diagnostics, EDI can also be used - electroodontodiagnosis, which allows determining the difference in the excitability of pulp tissues in its various states. Excitability is controlled by a special device with which a weak electric current is passed through the tooth.
Healthy pulp reacts at a current of 2-6 μA, but not more than 20 μA. Pulp gangrene reduces nerve excitability to 60-90 μA, depending on the percentage of cell death in the coronal part of the pulp and in the channels.

The doctor receives additional information in case of chronic gangrenous pulpitis during radiography of the tooth. The modern apparatus - a visiograph allows not only to obtain a contrasting and clear image of all tooth structures and surrounding tissues, but also to write these data to a computer disk.
A deep carious cavity, which communicates well with the pulp chamber, is usually visible in a photograph or a computer monitor in a diseased tooth. Sometimes, with chronic gangrenous pulpitis, changes in the tissues surrounding the tooth are recorded, for example, the expansion of the periodontal gap or slight destruction of the bone tissue around the apex of the tooth root.
Methods for the treatment of gangrenous pulpitis
The main method of treating gangrenous pulpitis is the so-called vital extirpation or, in simple terms, the complete removal (extraction) of the entire pulp from the root canal system. Since this form of pulpitis is irreversible, the biological method of treatment (conservative) is not suitable, since there is nothing left to maintain in a viable state.
For interesting details on the removal of the "dental" nerve, see a separate article:How to remove a nerve from a tooth and what problems may arise.
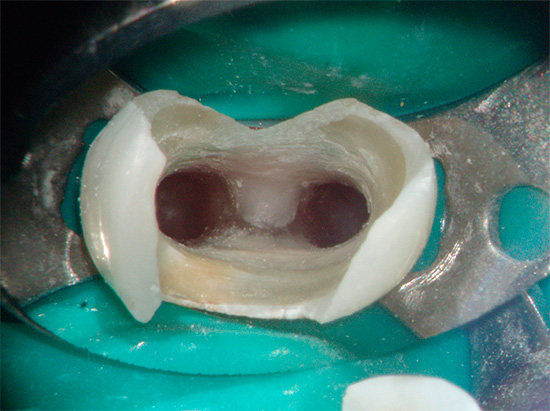
Photos of pulp residues removed from the root canal of the tooth:

For the same reasons, it is impossible to perform vital amputation while preserving only the root pulp, since it is almost always already involved in the processes of necrosis.
From the experience of the dentist
It is possible to use the pulp removal method with preliminary formulation of a devitalizing paste containing arsenic and without it, but with great care.Since it is often not possible to accurately determine the depth of death of a “nerve”, the thoughtless closing of a deliberately nearly dead tooth with a strong paste with a bandage often leads to complications in the form of severe pain.
And this is quite logical when it comes to the exudation phase against the background of a putrefactive process. If there is appropriate evidence or a desire to establish a devitalizing paste in the first visit, you should make sure several times that it will cover the root part, but the living “nerve”. It is important to keep in mind the criteria for the time it was on the tooth, since drug manufacturers calculate the average time, given that almost all pulp is alive, and in the case of chronic gangrenous pulpitis, an individual approach is required taking into account the amount of soft tissue that is not affected by necrosis inside the tooth.

Treatment of chronic gangrenous pulpitis involves several main stages:
- Anesthesia If an injection with an anesthetic is done at the level (in projection) of the roots of the diseased tooth, then the anesthesia is called infiltration, and if the entire nerve trunk is “frozen”, then it is conductor.
- Tooth isolation with a cofferdam prior to preparation or the use of sterile prefabricated or pre-twisted cotton rollers during canal filling and filling.
- Dissection of the carious cavity and mechanical removal of the "dirty" infected and pigmented dentin with drug treatment with antiseptics (chlorhexidine, hydrogen peroxide).
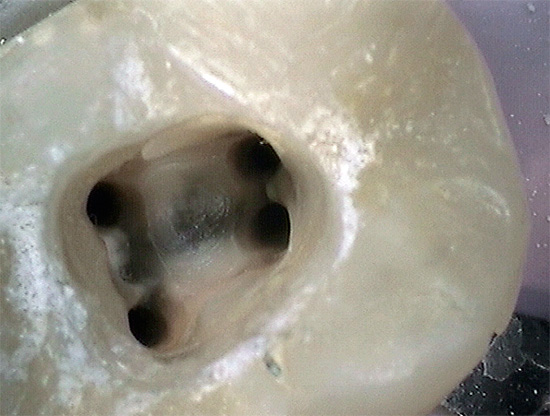
- Disclosure of the mouth of the channel.
- The passage of the root canals with files (special intra-channel "needles" with cutting edges), followed by expansion and the formation of a conical shape of the desired diameter. During the procedure, the obligatory washing out of the canals of the remains of pulp, pus, dirty sawdust from the walls, etc. is carried out. Modern dentistry has different methods of “washing” the canals, but jet lavage with sodium hypochlorite solution has become widespread with gangrenous pulpitis and its other types.
- Setting special anti-inflammatory, antibacterial and antiseptic pastes (only if indicated) for several days before the final filling of the canals.
- Determination of the length of the root canal by special devices (apex locators) or using X-rays using files or gutta-percha pins.
- Drying the canals and filling with hardening pastes or combining them with primary hard materials (gutta-percha pins).
- Quality control of filling channels using a visiograph or contact "film" radiography.
- The restoration of the function and aesthetics of the tooth with the help of modern filling materials (composites) is almost always carried out at the next visit, since the material in the canals should completely harden within a few days.



Drugs for the treatment of canals with gangrenous pulpitis
Despite the fact that in chronic gangrenous pulpitis, prolonged treatment of the canals with files and thorough medical cleaning with hypochlorite solutions with and without activation of ultrasonic devices with a laser are used, a number of dentists are of the opinion that to prevent the persistence of a residual infection near the root apex and reduce the risk of recurrence of the infection process , it is necessary to put an anti-inflammatory and potent antibacterial drug for several days before the final filling of the canal the drug.
From the practice of the dentist
For temporary filling of infected canals with gangrenous pulpitis in order to increase sterility, the drug "Gangraena-Merz" is used. This is a material based on calcium hydroxide, which creates a high pH level (up to 12), at which most microbes die in the most remote corners of the canals.However, you should not rely only on the unique positive properties of preparations based on calcium hydroxide, since an integrated approach for preserving the tooth is important: thorough thorough cleaning of the canals and their irrigation (irrigation) with disinfectant solutions, and only then, application for several days (up to a week) “ Gangraena-Merz "or its analogues.
At a budgetary reception in a hospital or clinic, dentists can not always thoroughly process the canals with gangrenous pulpitis in one visit, because the treatment is stretched for 2-3 visits when one or two antiseptics are used in turn. To date, the preference for the chronic gangrenous form of pulpitis is given not to pastes for intracanal treatment of pulpitis and periodontitis, but to liquids.
This is a kind of economical option that allows you to use affordable bactericides for as long as possible. The most effective and affordable means include Krezofen.
It is interesting
Kresofen is a bactericidal preparation based on dexamethasone, parachlorophenol, thymol and camphor for effective antiseptic treatment of channels. After removing the decay products of the pulp from them and washing them in the usual way, as well as after drying, a drop of Krezofen is placed in each channel. It is capable of easily penetrating in difficult passable areas in a short time, creating sterility in them.
To improve and consolidate the results, Krezofen can be left on cotton turunds for several days under an airtight temporary dressing, which creates maximum sterility and ensures the prevention of possible complications due to residual infection. On the next visit, it is enough to just dry the canals from Krezofen and seal them in an affordable way.

Treatment of gangrenous pulpitis in children
Children's dentists are of the opinion that with pulp necrosis in milk teeth everything should be done “in an adult way”: remove the decaying pulp, clean the canals and rinse them from infection, followed by filling in one or several visits. However, children always make their corrections not only by their behavior, but also by the peculiarities of the structure of primary teeth, the likelihood of an unformed and not closed apex of the tooth root or partially absorbed root during a physiological tooth change.
As a result, the pediatric dentist chooses a method of treating chronic gangrenous pulpitis, based on the individual characteristics of the child, the characteristics of the milk or permanent tooth, as well as the level of equipment of the clinic and its professional skills.

Since it is not possible to choose a biological treatment method and vital amputation due to the far-reaching necrosis of the pulp tissue, either the vital (devital) extirpation method with full pulp extraction or the long-used method of devital amputation with mummification of the root pulp after it is chosen for milk teeth killing.
More often, drugs based on resorcinol-formalin paste are used for this. Depending on the specific composition and manufacturer, they can be more or less toxic, but, in principle, contain the same basic components for mummification of a dead “nerve” and preservation of the tooth until it is changed. At the moment, Russia uses the Swiss Mummifying Paste (Mummifying Paste), Foredent (Czech Republic), Resodent (Russia), Endoform (Poland) and their analogues.
It is interesting
Around 1912, the German physician Julius Albrecht proposed the resorcinol-formalin method, the debate around which has not subsided so far. The “father” of one of the most popular and cheapest methods of root canal treatment worked as a dentist until the end of his life, without becoming either a professor or even an assistant professor.Little is known about his biography, there is no exact date of birth and death. It is believed that, most likely, the scientist was killed by hunger and disease.
Since the creation of the method, there has been debate around the validity and effectiveness of its application, there have been opponents and supporters among young and old professors and scientists around the world. For ease of use and cheapness, he was awarded the honor of widespread use for all groups of teeth, but no one thought about its negative properties then. Tooth staining in shades of pink until recently, few people were embarrassed, and the prospect tooth extraction after 5-10 years or more, she stopped no one: neither doctors nor patients.
Photo of a tooth cured of pulpitis using resorcinol-formalin paste:
Cost of treatment
Chronic gangrenous pulpitis is usually treated in two to three visits. In clinics, pricing is based on the level of the institution, professional equipment, doctors' qualifications, number of staff, treatment method, material used, number of visits and other factors. The price list usually indicates each procedure performed during treatment.
The pricing principle for the treatment of pulpitis can be traced according to the following standard scheme, in which payment is made for the following stages:
- anesthesia (some firms plus every injection of anesthetic);
- passage and washing of each channel separately (if there are 4 in the tooth, then the price for these manipulations increases 4 times);
- filling each channel with a specific material (large companies offer a choice of both "simple" filling cold gutta-percha with pastes and three-dimensional filling of hot gutta-percha "Termafil", which is much more expensive);
- the use of ultrasound or a laser to activate antiseptics in the processing of channels (some companies include this section in the payment for passage and washing of channels);
- The filling with which the treatment is completed (among the light-cured composites there are economy and business-class materials, which is prescribed in the price list).
If the dental clinic charges each visit, then each of these sections selectively appears in the receipt for payment of services. Naturally, if you need to pay, for example, 2-3 thousand rubles for a light cure with anesthesia, then the rest of the procedures can result in a tidy amount, since the standard flushing of one channel costs an average of 1000 rubles (for a 4-channel - already 4 thousand turns out).
For additional "options" the company sets the price in an arbitrary way - somewhere more, somewhere less.
It is not difficult to calculate that for one visit, in which all four channels of the molar (upper or lower) with gangrenous pulpitis will be passed and sealed, the cost of treatment will be about 7-8 thousand rubles, and the final seal is another 2-3 thousand, if you take average cost of treatment. In other words, the smaller the channels in the tooth, the cheaper it will be to treat pulpitis.
See nuances for an example. treatment of pulpitis of a three-channel tooth.
In many private clinics, dentists are directly interested in stretching the treatment of pulpitis for several visits in order to increase the cost. Moreover, the level of modern dental institutions allows creating such sterile conditions in the canal system and closing the tooth so tightly from the external environment until the next visit that the uselessness of re-washing the canals for the doctor is obvious, but the patient is not even aware of this.
What the clinic is capable of doing in one visit can stretch to several expensive procedures, since chronic gangrenous pulpitis is often positioned for the patient, as periodontitis has begun - inflammation in the root, which must be treated in several visits, using complex technologies and is necessarily expensive.
In contrast to commercial firms, state-owned dentists, on the contrary, underestimate the importance of flushing the canals and rarely use their blasting, limiting themselves to manual routine flushing with antiseptics on cotton turunds. As always, the hardest part is finding a middle ground ...
Be healthy!
Interesting video: an example of the treatment of purulent pulpitis of a molar (chewing tooth)
In detail about the mechanism of pulpitis development and features of its treatment


I do not agree that the doctor is interested in stretching the treatment because of material benefits, because it is completely unprofitable! Because it is important not how much one patient will pay in general, but how much is paid for one visit.
Maybe you did not carefully read the last block: it says that "many private clinics", but not all. Often, reviews are received from patients who, for each visit, wind up even with pulpitis. I’ll generally keep silent about periodontitis - this is fertile ground for the promotion for each new visit. We have a huge country, and where and how is done, you yourself can find out if you take a closer look at the features of private dentistry in different regions.