Chronic fibrous pulpitis is most often the result of acute pulpitis forms. However, sometimes the primary chronic course of the disease is possible, when the phase of acute inflammation is short-lived and goes away without the classic signs associated with severe pain.
The chronic form is a kind of compensation when fibrous degeneration of pulp tissue (“nerve”) occurs with minimal exudation, that is, the formation of fluid in the channel. In this case, fibrous connective tissue grows inside the tooth canals with a corresponding decrease in pulp sensitivity.
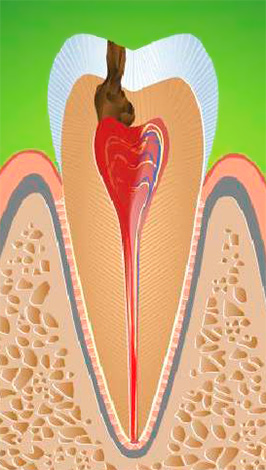
Structural changes in the pulp without decay and the formation of pus are the result of the reactivity of the body, when the state of inflammation of the tissues of the "nerve" allows you not to feel acute pain. In most cases, this contributes to tooth decay up to the pulp chamber, when the outflow of excess fluid from it occurs through an opening in the cavity.
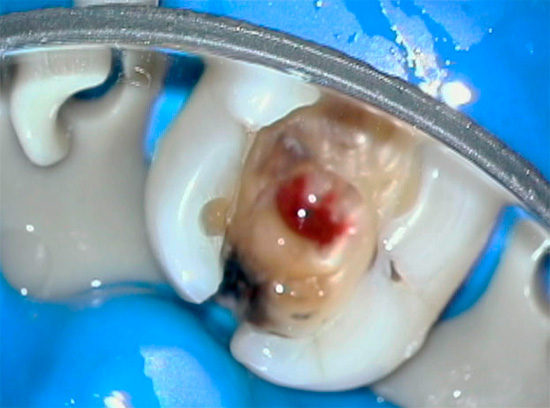
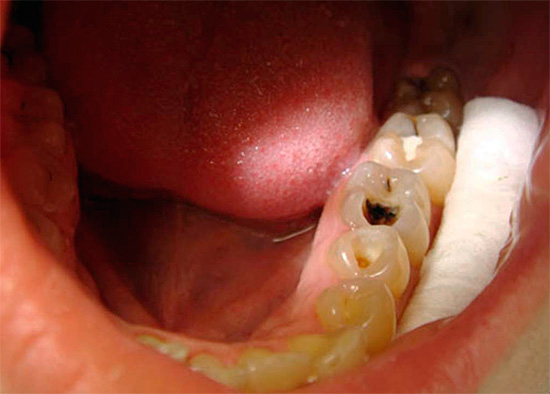
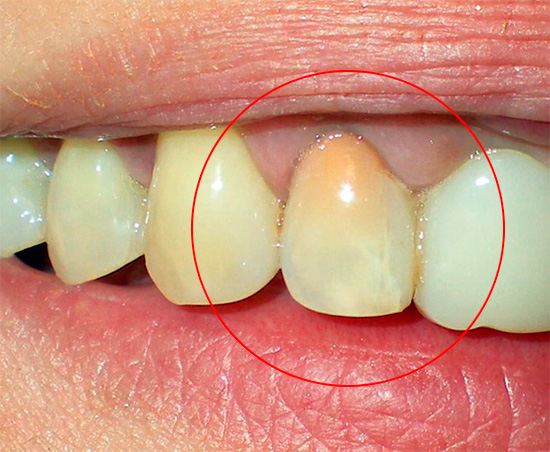
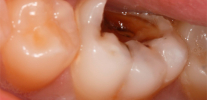
Photo of a tooth with a deep carious cavity reaching the pulp chamber:

See also article: What tooth decay may look like: photos.
However, with chronic fibrous pulpitis, despite the absence of acute pains, there is no need to talk about the well-being of the tooth. And the condition is in most cases temporary, since sooner or later a part of the pulp can die with phenomena gangrene "nerve"or necrotization of the entire pulp with the passage of purulent inflammation to the tissue surrounding the root.
The acute purulent process, in turn, can spread under the periosteum and cause a "flux", which often leads to tooth extraction. Generally speaking, the transition of the fibrous phase into pulp gangrene in all senses is unpleasant: a putrid odor from the mouth appears, the tooth turns gray, reacts strongly to hot, and additional risks of serious complications appear.

That is why it is so important to begin treatment of fibrous pulpitis as soon as possible, even before the transition of the chronic form of the disease to acute.
The history and dynamics of chronic fibrous pulpitis
Chronic fibrous pulpitis among other forms of pulpitis occurs most often and has a characteristic medical history. Usually a person is bothered by aching pains from various types of irritants (cold and hot food), which do not go away for a long time even after eliminating the source of irritation. Often aching pains are felt in those cases when the ambient temperature just changes: for example, when moving to a warm room from the cold.
In the presence of deep carious cavity, which communicates with the pulp chamber, pains may not bother or appear only when chewing hard food due to mechanical irritation of the "nerve". Similar case histories with chronic fibrous pulpitis are observed in the case of the location of the carious cavity beyond the access of irritants, for example, under the gum (root caries).

Why do aching pains prevail in the evening and at night?
Indeed, it is known that toothache manifests itself brighter in the evening and especially at night. Despite the fact that with chronic fibrous pulpitis there are only mild aching pains, however, in the evening and at night they often become more intense.
There are several versions about this. According to the first of them, night pains are associated with the fact that during the day a person is active and against this background he does not pay attention to mild pain, and in the evening and at night the body relaxes and pains are felt more acutely.According to another version, night pains are due to the fact that the nerve branches associated with the vagus nerve approach the tooth, and night has long been called the “Vagus kingdom,” that is, an increase in the activity of this particular nerve, so the tooth hurts more precisely at this time. For dentists, however, the explanation is closer, due to the fact that in the evening and during sleep, metabolic processes weaken, the outflow rate of toxins from the pulp decreases, which causes its swelling and compression inside the tooth. Since the pulp is a neurovascular bundle, its prolonged compression causes severe pain.
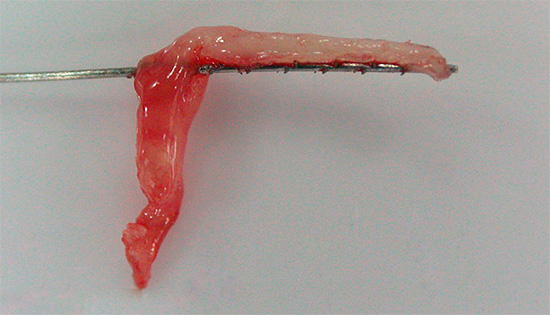
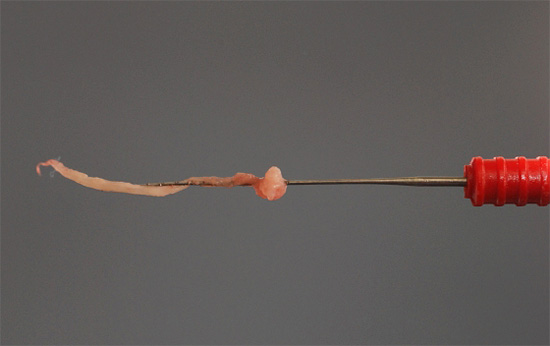
Photo of pulp removed from a tooth:
Case from practice.
A 42-year-old man came to the dentist with complaints of a carious cavity in the upper left tooth, due to which there are aching pain when eating, as well as a gradual increase in pain from cold. The patient focused on the violation of the gap between the teeth, since during food there is pain in the gums and you have to remove the remnants of food with toothpicks.
From the medical history: about a month ago, acute paroxysmal pains appeared in this tooth, which the patient removed Ketorol painkillers.
Objectively: upon visual inspection, a deep carious cavity filled with softened and pigmented dentin is determined in the upper left fifth tooth (2.5). The medial contact wall and chewing surface of 2.5 teeth are destroyed by a carious process. When probing, the opening point of the tooth cavity is determined, in which the pulp is visible. When the probe touches at this point, the pulp bleeds painfully.
To clarify the diagnosis, percussion of the tooth, EDI and radiography were performed. With tooth percussion, there is no pain, the EDI data is 40 μA. On the x-ray there is a message of the carious cavity with the pulp chamber, no changes in the periapical tissues were detected.
Diagnosis: chronic fibrous pulpitis 2.5 teeth.
Treatment:
- infiltration anesthesia with SEPTANEST 1: 100,000 (1.7 ml) was performed in the projection of the tops of the roots of 25 teeth on the gums;
- preparation and machining of the carious cavity from softened dentin;
- drug treatment with 2% chlorhexidine;
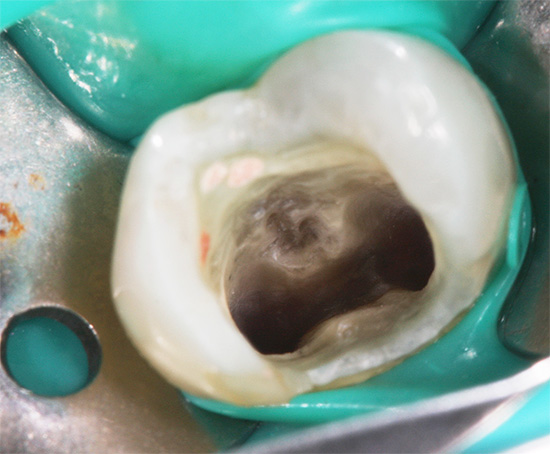
- opening fissure boron access to the mouth of the root canals:
- amputation of coronal pulp;
- extirpation of the root pulp by a pulp extractor;
- opening of the mouths of the medial and palatine canals with Gates Glidden burs;
- establishing and fixing the working length of the channels;
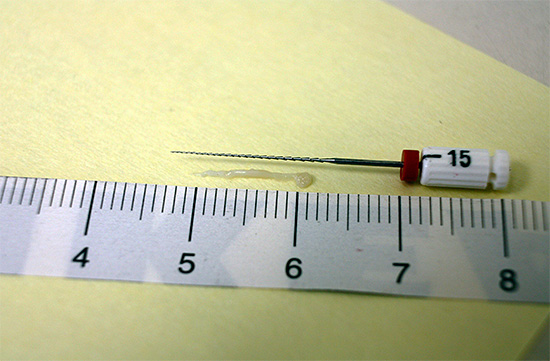
- passage and expansion of channels with K-files from No. 15 to No. 40 with alternating drug-jet treatment of channels from an endodontic syringe with 3.25% sodium hypochlorite;
- drying the channels with paper pins;
- apex locator control of channel lengths;
- filling channels for a given length using cold lateral condensation of gutta-percha (No. 35-40, 4 taper) with Endometasone N.
A temporary Light Clip cure filling is installed on the tooth. The patient is scheduled for the next appointment after 3 days.
Repeated reception. A temporary dressing was removed, and the walls of the cavity were corrected. The open sandwich technique was used: a sectional matrix was installed between 2.4 and 2.5 teeth with wedges to restore the medial contact point.
Vitrebond glass ionomer cement of light curing was added to the bottom to the enamel-dentin border, the aesthetic and functional properties of the tooth were restored with Filtek Z-250 light curing restoration, grinding and polishing with disks, polishes, brushes with Detartrine Z paste.
The control of the installed seal is scheduled in a week.
Diagnosis of chronic fibrous pulpitis
The diagnosis of chronic fibrous pulpitis is finally made only after appropriate confirmatory studies.
Usually in the tooth there is a deep carious cavity with softened infected dentin, which often communicates with the pulp chamber.To clarify the presence of such a through message, the dentist uses a probe - a curved and sharp metal instrument at the end that probes.
During this procedure, it becomes clear whether there is a message on the bottom of the cavity with the pulp of the tooth. If there is a message, then after sensing the pulp often begins to bleed painfully.

It is interesting
Currently, dentists rarely resort to the method of deep sounding for reasons of humanity, or they implement it very carefully. The older generation can tell a lot of stories that an unscrupulous dentist during the diagnosis “poked” a tooth with something sharp so that “sparks fell from his eyes”. Such cases, unfortunately, are recorded today, especially at the reception in budgetary clinics.
Practice shows that severe pain during the sensing procedure occurs when the tip of the probe places excessive pressure on the bottom of the cavity against the background of acute pulpitisrather than chronic. As a rule, in the chronic form, probing the “nerve” already injured with food does not bring unbearable pain, although modern dentists, given the human diagnostic methods, refuse this risky method.
Palpation of the gums near the diseased tooth is always painless, and percussion (tapping) on the pulpitis tooth with the blunt end of the probe or dental mirror does not bring pain.
One of the important stages of diagnosis is also thermometry - determining the reaction of a tooth to temperature stimuli. So, for example, if, when a tooth is exposed to cold water when it is supplied from a syringe with a blunt needle, the pain does not go away for a long time even after eliminating the irritant, this indicates a living “nerve” inside the tooth and its chronic inflammation.
As part of the differential diagnosis, electroodontodiagnosis (EDI) is perhaps the most informative method, and allows you to accurately determine not only the chronic stage of inflammation with fibrous degeneration of tissues inside the tooth, but also to distinguish it from other chronic forms (pulp gangrene and its hypertrophy). Since a healthy pulp begins to respond to a current of 2-6 μA (with deep caries - up to 20 μA), all serious deviations from this value indicate a particular state of pulp inflammation. With fibrous pulpitis, the "nerve" responds with excitement and pain with a current strength of 35-50 μA.
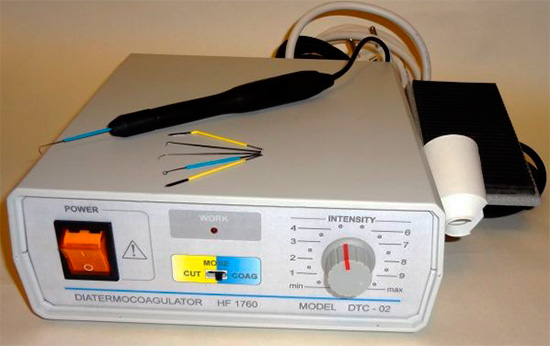
The photo below shows a device for conducting electrical diagnostics:

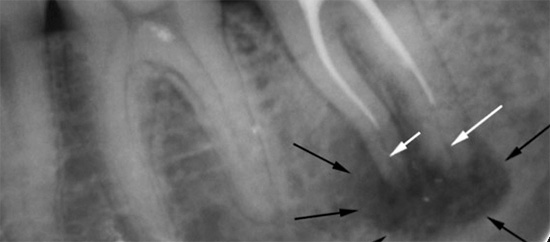
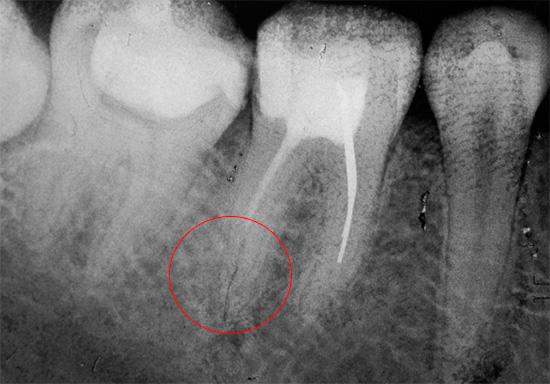
X-ray diagnostics is also important. In chronic fibrous pulpitis, a deep carious cavity, which almost always communicates with the pulp chamber, can usually be observed on the radiograph of a diseased tooth. Sometimes a slight expansion of the periodontal gap (the space between the root and the bone of the alveoli in which it is fixed) is fixed.
Differential diagnosis of chronic fibrous pulpitis is carried out with deep caries, acute pulpitis and chronic gangrenous pulpitis. It is with these diseases that fibrous pulpitis is most similar.
Deep caries never communicates with the pulp of the tooth, and probing is painful along the bottom, and not at one point. The pain quickly disappears when the irritant is eliminated, in contrast to fibrous pulpitis. Indications of EDI for deep caries are not more than 20 μA, and for fibrous pulpitis from 35 μA.
The acute form of pulpitis is easily confused with the chronic. The most differences are revealed when studying the history of the disease, since with chronic fibrous pulpitis there are no complaints of acute spontaneous pain and pain radiating somewhere (to the temple, ear, nape, etc.). The patient indicates that all these signs used to be, but over time they disappeared and only prolonged aching pains remained. When probing the bottom of the cavity in the background acute pulpitis most often there is no communication of the carious cavity with the "nerve", in contrast to fibrous pulpitis.

Gangrenous pulpitis (pulp gangrene) can be confused with fibrous, but its fundamental difference is the appearance of the tooth (grayish tint), putrefactive odor from the cavity, tooth decay to the mouth of the canals and pain when probing the canals. Also, the leading indicator in the diagnosis in this case is the EDI data, which reach 60 μA with pulp gangrene.
Surgical treatments for fibrous pulpitis
Since fibrous pulpitis is an irreversible inflammation of the pulp tissue, the treatment involves surgical intervention: partial or complete extraction of pulp from the canals. You can read about the exciting nuances of this procedure here: How to remove a nerve from a tooth and what problems may arise.

It is interesting
Literary sources at the end of the last century inform that with chronic fibrous pulpitis a biological (conservative) method of treatment can be used, however, most practicing authors of modern scientific papers have come to the conclusion that the effect of such treatment is very doubtful, and the prognosis for the future is not favorable. Structural changes in the pulp tissues do not allow it to return to its previous state even due to strong drugs based on antibiotics and calcium hydroxide.
Partial pulp removal as a method of treating chronic fibrous pulpitis is extremely rare, since it is difficult to diagnose whether there are serious fibrous changes in the root pulp. After all, it is the root pulp with this treatment method that is saved and drugs are put on it to relieve inflammation. The difficulty of maintaining perfect sterility in the work area and the possibility of repeated inflammation of the pulp residues does not allow dentists to hope for success from this type of treatment, and the prospect of redoing the work again determines the choice in favor of the method of completely removing the pulp from the root canal system.
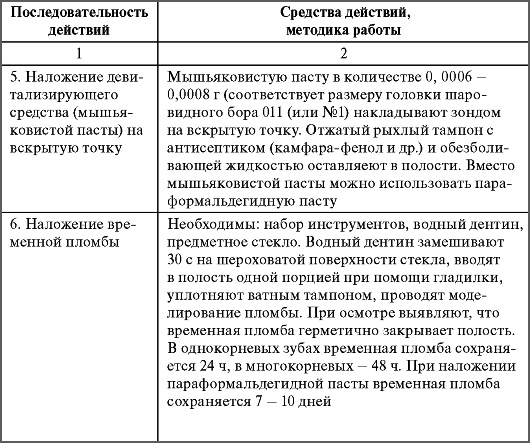
Complete extraction of pulp from the root canals allows you to reliably rid the tooth of the source of infection that provokes pain in the tooth. To do this, apply the method of simultaneous extraction of the "nerve" followed by purification of the canals with antiseptics, or with preliminary devitalization (killing) of the pulp using arsenic paste or arsenic-free analogues.

It is interesting
Thanks to not the most competent explanations of dentists, people still believe that after the first visit to a doctor in the treatment of pulpitis, a “medicine” is first established in the tooth. For those who were unlucky with the doctor, such a “medicine” also causes severe pain, as it turns out that this arsenic paste was improperly installed in the carious cavity and instead of killing the pulp only irritates it very much. Such a paste, of course, does not carry any properties of the medicine, and sometimes in the hands of an inexperienced dentist it becomes poison for the tooth and the body as a whole.
Modern dentists for the treatment of chronic fibrous pulpitis of any tooth choose the method of complete extraction of pulp from the canals under effective anesthesia. After a good “freezing”, the coronal part of the “nerve” is first removed, and then the root is removed with the help of pulp extractors (thin needles that allow the pulp to be removed due to special hooks). After that, the dentist conducts the passage and expansion of the channels with files (tools that have cutting edges and a handle for holding), together with the drug treatment of all the channel branches with antiseptic solutions.
Usually, treatment of chronic fibrous pulpitis takes 1-2 visits, depending on the tactics of the doctor.In certain clinical situations, the dentist can put solutions or pastes with strong antiseptics into the canal system to improve channel sterilization and prevent exacerbation in an already dead tooth, so an additional visit appears.
Features of the treatment of fibrous pulpitis of primary teeth in children
For the treatment of fibrous pulpitis in children today, different methods are used, depending on:
- level of dental organization (budget or private);
- clinical case (roots are formed or not);
- professional dentist
etc.
Most often for the treatment of fibrotic pulpitis of primary teeth with formed roots, a technique is used that does not differ from that in adults. The only distinguishing point is that in children, due to the specifics of the treatment (excessive activity and timidity), paste is often placed for preliminary devitalization of the pulp (usually non-arsenic) to prepare for extraction at the next visit.
On a note
As a devitalizing paste in children, for example, Devit-C is used, or - a potent devitalizing paste that does not contain arsenic. As an active substance, it contains paraformaldehyde, which reliably "kills" the pulp. To set this paste for chronic pulpitis in a milk tooth, it is necessary to open access to the pulp chamber well. Usually a paste the size of a millet seed is sufficient, but for multi-rooted baby teeth, the dose is increased individually. Pasta is put on average for 3-5 days, and sometimes up to one week.
Due to the fact that children most often do not fully carry out all manipulations for canal treatment, which requires a lot of time to achieve a positive result, pediatric dentists, especially in budgetary clinics, sometimes choose methods of devital amputation, that is, removal of coronal pulp after devitalizing paste and mummification of the root. Preserving the “dead” root pulp after the use of potent mummifying agents is a rather risky event, since the mummified "nerve" can cause chronic inflammation in the root, up to the appearance of fistulas on the gums or cysts on the root of the milk tooth, and this will directly or indirectly affect the rudiment of a permanent tooth.
Additional information can be found in a separate article: Treatment of pulpitis of deciduous teeth in children.
From the experience of the dentist
In some dental clinics, resorcinol-formalin paste and its analogues in the form of finished preparations, which are prohibited in all countries except Russia, are still used as mummifying agents. Teeth (milk or permanent), cured by this method, look, to put it mildly, not very beautiful: after some time, the entire crown part of the tooth is painted in a shade of pink or red, which is very striking to others if the treated tooth is in the smile zone.

Problems that may arise during treatment
During treatment of pulpitis, there may be both mild and severe complications. Mild complications include those that are easier to fix and which are not so dangerous for human health and life.
For example, the most common mistakes in the treatment of fibrous pulpitis are underfilling of the tooth canals. The quality standard for treating canals provides for filling them over the entire length tightly and to the apex - physiological constriction. If the canal is not sealed to the indicated mark, then in the future there may be big problems associated with the activation of infection in the voids of the canal. It is especially dangerous when the channel is sealed only 20-50%.
Moreover, dentists are faced with situations where in the budget (free) dentistry they do not fill the canals at all or do them with pastes, which are spread on the walls of the canals, posing as a finished treatment. Naturally, in almost 100% of cases, their colleagues redo the work because of the pain or discomfort after improper treatment.
It is most difficult to correct the error associated with the removal of filling intracanal material beyond the root.Sometimes this mistake is worth the patient’s health if the material goes deep into the maxillary sinus (when treating the canals of the upper tooth), or into the mandibular canal (when treating the lower tooth).
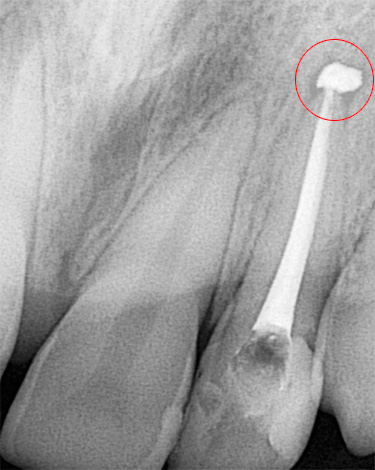

In such cases, the removed filling material acts as a foreign body, irritating the tissues and provoking severe pain. Sinusitis develops in the maxillary sinus, and neuritis develops in the maxillary canal. Timely help in the form of surgical intervention by a dentist-surgeon to extract excess material saves health and often life to the patient. For obvious reasons, a tooth with such a complication often has to be removed to provide better access to foreign material.
Physiotherapeutic treatment
Physiotherapeutic methods for treating fibrous pulpitis are used both during and after treatment. During canal treatment, for example:
- diathermocoagulation of the "nerve";
- transcanal electrophoresis of iodine.
Diathermocoagulation is the denaturation of the pulp protein or, in other words, its thermal coagulation. Due to the very heated tip of the needle introduced into the canal, heat is generated, which produces pulp necrosis in a matter of seconds (2-4 seconds), thereby reducing the risk of bleeding when it is removed. Also, microorganisms die, which prevents the penetration of infection beyond the root.
Transcanal electrophoresis of iodine: this method is used in poorly passable channels with a bactericidal purpose, that is, to destroy microbes in hard-to-reach places. This technique allows avoiding future risks of complications in the form of apical periodontitis - inflammation of the tissues around the root.
If post-filling pain is worried after the completion of the canal treatment, but there are no signs of serious errors in the image that require correction, then anesthetics electrophoresis, ultrasound therapy and laser, as well as microwave radiation are used. All this allows you to quickly remove traumatic pain.
To summarize a short summary. Timely seeking help for chronic fibrous pulpitis allows you to avoid future complications in the form of gangrene of the "nerve" with subsequent purulent fusion of it, which means to save the tooth from removal. Thanks to modern advances in dentistry, today it is possible to completely painlessly treat canals with a long-lasting and aesthetic filling. So it makes no sense to endure pain and drink it with painkillers, it is much easier to cure a tooth and sleep peacefully.
Useful video: what is important to know about pulpitis
Pulpitis treatment under a microscope


My son was diagnosed with a paid appointment in a dental clinic: chronic fibrous pulpitis of one of the teeth. At a budget reception, this tooth is designated as caries. Who to believe?
Hello Olga! Given the scarcity of your data, you asked a highly provocative, controversial question.On the one hand, one would think that at a budgetary reception, the complication of caries — fibrous pulpitis — was negligently overlooked, since there is little time for detailed diagnosis and there is no desire to tinker with several stages of treatment. On the other hand, a paid clinic is often interested in expensive intra-channel treatments. Unfortunately, fibrous pulpitis does not always have symptoms, so it is important to see how damaged the tooth is and whether there is a message in the carious cavity with the pulp chamber where the "nerve" is located. Sometimes a clue may be data on previously occurring acute pains, which gradually turned into aching and prolonged. Any information that can confirm a particular diagnosis is important for further conclusions.