What is popularly called the dental nerve, in fact, is a neurovascular bundle, which has a rather complex structure and is correctly called pulp. Thanks to this tissue located inside the crown and root of the tooth, it is able to respond to external influences: for example, to feel hot and cold food. Pulp is also a kind of barrier to the further penetration of bacteria.
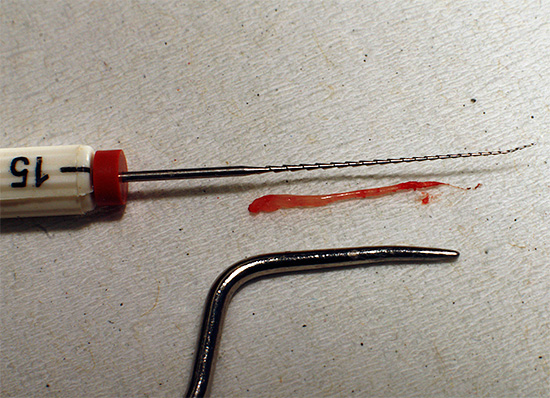
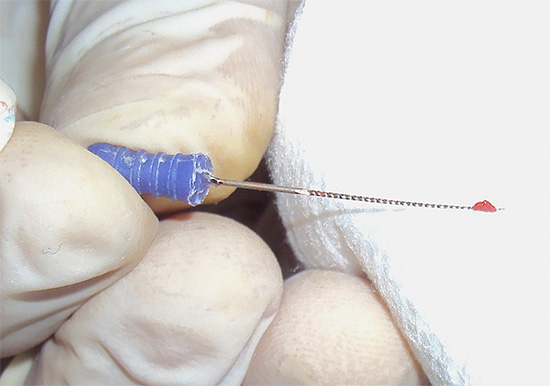
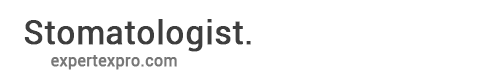
The photo below shows the nerve removed from the tooth:
Removing a nerve from a tooth causes it to become “dead” and lose its ability to perceive almost all types of stimuli (cold, sweet, sour, salty). But a tooth is called dead, first of all, for the reason that it loses its blood supply, the rate of mineralization processes decreases significantly in it - in other words, it becomes brittle over time, and the enamel becomes dull.
However, why then do dentists so often remove the nerve from the tooth, thereby actually depriving it of a very important internal component? What consequences can be prevented by this, and is nerve removal really necessary?

Next, we will try to consider these issues in more detail, as well as get acquainted with the patient’s reviews about the “unforgettable” impressions of the dentist and see how the nerve removal procedure can occur and in which cases it is sometimes accompanied by very, very unpleasant sensations ...
When you have to remove a nerve from a tooth
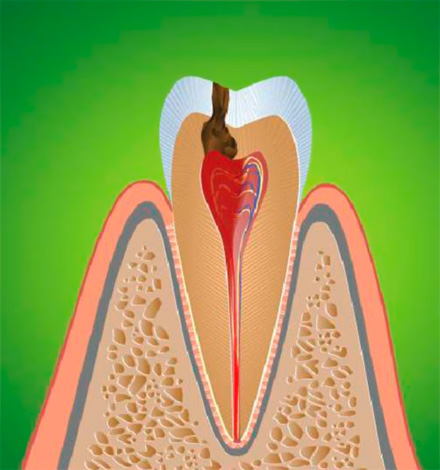
During initial tooth decay the nerve is not yet affected, but with deepening the carious process bacteria eventually penetrate into the pulp chamber, causing inflammation here - pulpitis. At the same time, a person can experience severe pain, often worse at night.
Pulpitis (inflammation of the tooth “nerve”) is a disease that almost always requires the partial or complete removal of the affected pulp from the tooth in order to avoid further spread of the infection beyond the root, which could lead to the development of serious complications.
Sometimes there are cases when nerve removal is required after a severe tooth injury, most often the anterior one. Traumatic pulpitis It is not as common as infectious pulpitis of carious origin, but it will still be necessary to remove the nerve from the tooth.
There are also known cases when an infection penetrates inside a tooth not through the carious cavity, but through the so-called retrograde route, that is, through an opening at the apex of the root. At the same time, the stages of the inflammatory process in the pulp go along the same principle as with classical pulpitis.
In rare cases, the pulp is damaged by calculi or "stones", sometimes under certain conditions appearing in the root canals and compressing the delicate tissues of the neurovascular bundle, causing their irritation. In this case, traumatic damage to the pulp may occur, followed by an inflammatory reaction, which leads to the need to urgently remove the nerve from the tooth, which often visually looks completely healthy.
This is interesting: "Do I need to remove the nerve from the tooth before prosthetics with crowns?"
Depending on the clinical situation, the orthopedic dentist can direct the patient to the dentist before the preparation of the tooth under the crown, who will remove the nerves from the tooth, clean the canals and fill them to the apex. With a badly damaged tooth under the crown, nerves are necessarily removed, and in cases of prosthetics with cermet - this depends on the tactics of the doctor.
There are two schools or two approaches to metal-ceramic prosthetics: either leave the pulp in the tooth or completely remove it.Moreover, if the orthopedic dentist chooses the latter option, this does not mean that he is a bad doctor. The fact is that a large part of the tooth is “cut” under the cermet, and the likelihood of overheating of the nerve or its damage during this procedure is extremely high. Therefore, by balancing the risks, the dentist can decide not to jeopardize future prosthetics and eliminate uncertainty: does the tooth ache under the crown or not.
A different opinion is shared by the school, which preserves the pulp in the canals during prosthetics with cermet. But this requires a high level of professionalism of the doctor (backed up by a special preparation technique), as well as the presence of certain equipment, allowing during the grinding to cool the tooth from all sides.
How painful is it to remove the pulp from the tooth?
Modern dentistry has methods that reliably anesthetize a tooth so that the removal of the dental nerve is painless. However, although this may seem strange, not all doctors are fluent in pain management techniques and not all clinics have effective anesthetics for local anesthesia. In some free clinics, the situation with this can be especially deplorable.

That is why reviews are still appearing that excite the minds of those people who are preparing for the first time to tooth removal (removal of the nerve with subsequent filling of the canals).
Feedback:
“About 10 years ago I was treating the lower chewing tooth in the polyclinic at the place of residence (free of charge, which I regretted). I already had experience when a nerve was removed from a tooth. I thought the doctor would put arsenic and all that. And he just drilled a tooth. Then he stuck something into it (already sparks from his eyes) and pulled out a nerve. Without any pain relief! Horror in general. "
Konstantin, Izhevsk
It is the panic fear of the upcoming nerve removal procedure that causes some people to take risks, turning to clinics where they are treated under general anesthesia, that is, with a complete loss of consciousness. Moreover, sometimes no arguments that most people receive absolutely painless help in treating pulpitis under local anesthesia (that is, in consciousness) do not help. Even the increased price of removing a nerve from a tooth under anesthesia is not an obstacle in such cases.

However, in addition to the desire, at your own peril and risk, to lie down on the "operating table" and remove nerves from one or several diseased teeth in a dream at once, there are strict indications for anesthesia, which a competent dentist must take into account when choosing methods and means of anesthesia.
Feedback
“I don’t know why people are so scared to go to the dentist to remove the nerves, but I personally had them cleaned more than once and there was no severe pain. With an injection there are no pain at all! For the thirty minutes that the doctor picks there, he can be pricked a couple of times, but this can’t even be called a pain. It’s just a feeling that they’re doing something in the tooth, and there’s no pain during the removal of the nerve. ”
Valentina, Neftegorsk
The main steps of the nerve removal procedure
Having decided on why the nerve is removed from the tooth at all (and that it doesn’t always hurt), we will move on to the next question: how does this procedure actually occur. What exactly can you expect in the dentist's office?

Generally speaking, depending on the nature and depth of the damage to the pulp tissue, the doctor can decide on the partial removal of the nerve (the so-called amputation) or its complete removal (extirpation). When a nerve is amputated, only the coronal part of it, which is located in the pulp chamber, is cut off, and the root part is preserved. However, this technique is not common, so most often resort to the complete extraction of the dental nerve from the canal system. And the more of these channels, the higher the price of treatment will be.
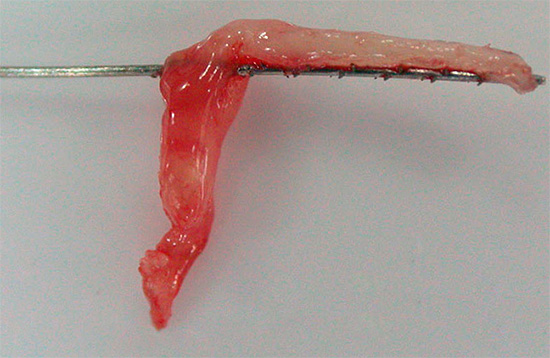
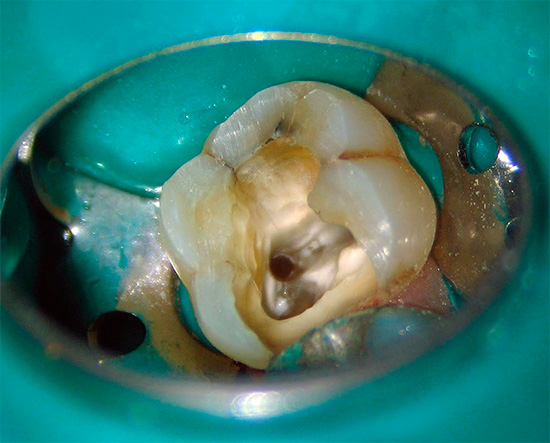
In the photograph below, the root canals are clearly visible - each of them must be thoroughly cleaned from the remnants of the pulp, otherwise the infection preserved in them can lead to serious consequences in the future:

For interesting details on the treatment of pulpitis in teeth with multiple canals, see a separate article: About the treatment of pulpitis of three-channel teeth and the prices for this procedure.
Consider the main stages of preliminary preparation for the procedure for removing a nerve from a tooth:
- X-ray of the tooth. It is used, for example, in case of any doubts of the doctor at the stage of diagnosis. If there is a suspicion that the nerve in the canals has died, then they often do intraoral contact radiography, or a picture on a visiograph, which is safer than the first option.
- Anesthesia. Local anesthesia is usually used, but, as noted above, with certain indications or wishes on the part of the patient, treatment can be carried out under anesthesia with a complete loss of consciousness (especially anesthesia is in demand in the treatment of young children). In the case of local anesthesia, techniques and anesthetics are used to remove the nerve, which allow reliable and long-term “freezing” of the tooth, almost completely turning off its sensitivity for a while.
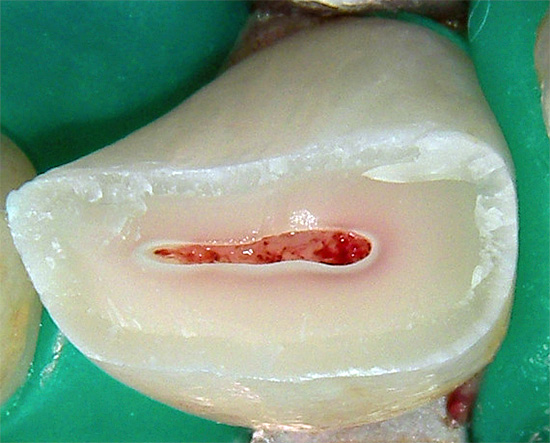
- Isolation of the working field. In expensive private clinics, before the treatment of the tooth, cofferdam is applied - a special latex film that protects the diseased tooth from saliva from entering the oral cavity and, in addition, creates more comfortable working conditions for the doctor.

- Processing of carious tooth tissues with simultaneous air-water cooling, creating convenient access to the pulp chamber, opening it and forming smooth vertical walls.
After a quality preparation, the nerve itself is removed from the tooth, which is performed by a pulp extractor - a special disposable tool. The structure of the pulp extractor allows you to capture the neurovascular bundle and remove it from the tooth canal after turning the tool along the axis by an angle of 90-180 degrees.
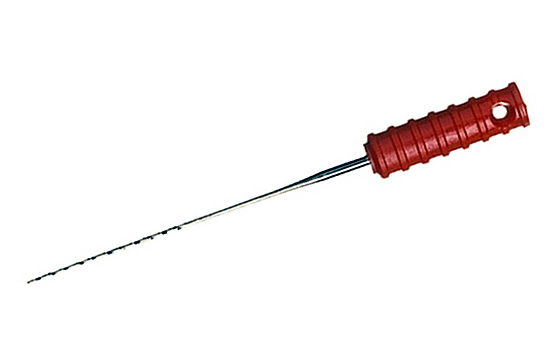
With a sufficiently wide channel, it is often necessary to introduce more than one pulp extractor to capture the pulp.
It is interesting
The prototype of the first pulp extractor was an ordinary piano string.
Currently, there is a technique for removing a dental nerve without a pulp extractor. Some dentists are of the opinion that in some clinical situations, the pulp extractor extracts the nerve too roughly, creating a traumatic separation of it along with periodontal tissues, which in rare cases can lead to certain negative consequences.
Therefore, universal files are used - tools for the passage and expansion of root canals, which allow you to accurately and controlledly cut the pulp along a given length without disturbing the surrounding tissue root sensitive to endodontic treatment. Control of nerve removal by this method can be carried out according to x-ray data, as well as special instruments for measuring channels, tables, etc.

Note: “Is it possible to remove a nerve at home and if so, how to do it?”
Unfortunately, the answer to this question that excites many people is only negative.
As practice shows, there are many "craftsmen" who, when acute pain they independently try to kill a nerve in a tooth at home, and if possible, get rid of it altogether. So, for example, there are cases when people “burned” their dental nerve garlic, with ammonia, acids, alkalis on a cotton wool, embedded in the "hollow", they tried to burn a nerve with a hot needle and even a spark from a car ignition system.
However, all these methods can not be called safe for health. And even if you get somewhere arsenic paste, which is intended only for professional use, then at best it will not remove the nerve, but will cause necrosis (necrosis), and in the worst - even more pain when the living nerve is intact, or in general burns gums around the patient and healthy neighboring teeth.
If the treatment of the tooth canals ended immediately after removal of the nerve, then this would greatly simplify the lives of both doctors and their patients. However, everything is somewhat more complicated.
In order to preserve the tooth for the rest of his life, immediately after removing the pulp from all the channels, the dentist passes and expands them along the given root length, thoroughly rinses them with active antiseptics (from the remnants of the infection and pulp) at these stages, seals them, and then makes a control shot .

A permanent tooth filling is installed on the first or (more often) the next visit.
(Visually some of the procedures for endodontic tooth treatment can be seen in the video at the end of this article).
Possible medical errors and their consequences
Removal of a dental nerve is a responsible event in every sense, on which the fate of an already dead tooth depends. Under certain circumstances (unprofessionalism or a doctor’s fatigue, outdated equipment and instruments), medical errors may occur during nerve removal, which sometimes lead to tragic consequences for the tooth.
Most often, two complications arise during pulp extraction:
- breaking of the tool in the channel;
- heavy bleeding from the canal.
The photo below shows an example of a broken dental instrument in a canal:
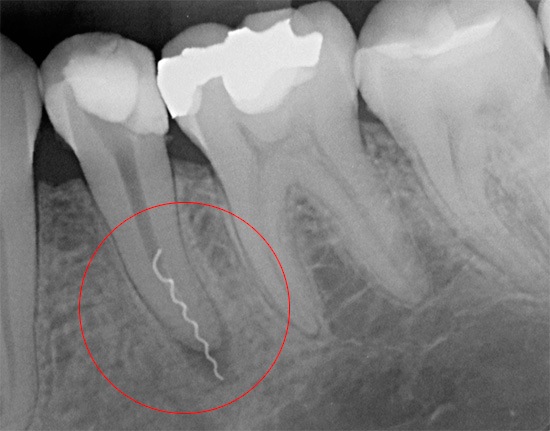
However, if breaking off the instrument can be called a classic doctor’s mistake, then bleeding from the canal can sometimes be difficult to foresee - for example, pulp detachment during pulp extraction can take place too deeply. That is why a number of dentists do not consider it advisable to take risks by removing the nerve from the tooth with a pulp extractor, and prefer another method: cut off the soft tissue gradually with files with copious step-by-step flushing of the canal with antiseptics.
The pulp extractor in the channel is broken off due to a violation of the technique of working with it (excessive torsion in the channel), or when using unsuitable (defective) tools.
If bleeding from the tooth canal most often stops quickly and does not have serious consequences, then extracting the left piece of pulp extractor is a complex procedure that requires the appropriate skills and certain equipment from the doctor. Leaving the “dirty” pulp extractor residue in the untreated canal means removal for the tooth - and this is only a matter of time.

Another possible complication due to the doctor’s fault is the reappearance of pain, which is the result of incomplete extraction of the nerve from the dental canals. Unfortunately, even at present, there are cases when a doctor, due to rush, negligence or fear of causing a person pain, may accidentally or intentionally leave a part of the dental nerve in the canals not removed.
It is no accident that the clinic even has a diagnosis of residual pulpitis, when an exacerbation of the repeated inflammatory process begins in a decaying nerve residue in one or several channels. In this case, after incomplete removal of the nerve, the tooth first aches, and then it can acutely ache with further spread of the infection to the tissues surrounding the root and the development of a more serious disease - periodontitis (in this case, patients may feel that the tooth pulsates from pain after removing the nerve).
With the development of residual pulpitis, it is necessary to urgently treat poorly treated canals again, since the completely not removed infected nerve poses a threat of serious complications, leading at best to tooth extraction.
Question to the dentist: “Why does my tooth darken after removing a nerve?”
After a quality treatment of the canals, the tooth usually does not darken over the years, but only grows darker, that is, it loses its natural luster, which is not a deviation from the norm.If the tooth turned black or yellow after some time after removal of the nerve, then you should look for the cause either in the preparation of the tooth cavity for filling (in poor-quality excision of carious tissues) or in poor instrumental processing of the canals while leaving nerve residues and bacterial infection in them.
In addition, often a serious change in the color of the tooth crown is associated with the material used for filling the canals. So, for example, some dentists by mistake still continue to fill the canals of the front teeth after removing the nerve with Endometasone, because of which after a few years the teeth can turn very yellow, which is even indicated in the instructions for the material.
All shades of pink can appear on a dead tooth after filling the canals with resorcinol-formalin paste. Unfortunately, they still continue to use this harmful paste in all senses at a budgetary reception, especially after removing nerves from deciduous teeth.

How much can a tooth treatment with nerve removal cost?
The price of removing a nerve from a tooth is formed taking into account each stage of the procedure and its complexity. Ah, if only the cost of removing the nerve from the tooth and anesthesia were recorded in the receipt for the services, then the treatment would be worth a penny ...
In fact, in the final list of services provided by the dentist, as a rule, at least 5-6 points of the price list appear: from anesthesia and the passage of each channel with its filling to the cost of the final seal.
Here is a photo with an example of a price list for pulpitis treatment services (caries complication):
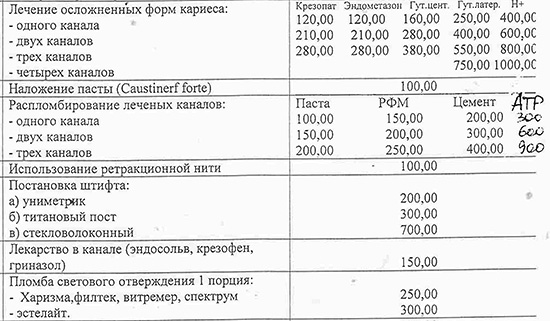
A person who is not familiar with dentistry usually cannot clearly figure out how much it will cost to cure a tooth with removal of a nerve and setting a permanent filling. And even often the administrator of the clinic, not knowing the nuances of endodontics, can only very roughly tell the price.
Therefore, most often the patient is informed of the minimum possible amount. As a rule, this is a single-channel pulpitis, the treatment of which should take place without force majeure (without narrow and curved channels, without the use of additional drugs and x-rays).

On a note
When the consultant tells you the price, for example, “from 3000 rubles”, and after treatment the receipt consists of 8-10 points with a final amount of 10,000 rubles, then, friends, you should not immediately suspect the clinic employees of fraud. It is possible that you should be offended only by your sixth upper tooth with five narrow channels, which the doctor had to go through for more than 2 hours, expand and wash with ultrasound activation, constantly take intermediate pictures on the visiograph, and in the end - seal them with the Thermafil system ”And install a high-quality“ light ”seal with a 5 year warranty.
Fortunately, there are clinics and highly qualified doctors who pre-negotiate the cost of treatment with patients based on a free hour and more consultation and diagnosis. In such cases, a fixed price is not set, but a range of deviations from the final cost is not too blurred, for example, from 8 to 9 thousand rubles for a full treatment of the upper sixth tooth after diagnosing the maximum of possible nuances (surprises) for the future.
Interesting video: close-up dental nerve removal
And here you can see all the stages of treatment of pulpitis of a single-channel tooth





Today I went to the dentist. I treated two front teeth (for a fee), an injection is the most painful thing I felt during this hour. During the removal of caries, the nerve was affected and it had to be removed, it didn’t hurt, I didn’t feel anything - neither my teeth nor the tip of my nose. Everything went well, but the doctor said that the tooth may darken over time and will hurt for a month, it was this news that really upset me.
Just came from the dentist. She treated one front tooth (broke it). It was simply not possible to increase it, since the cleavage was more than half of the tooth, it was necessary to remove the nerve, put the pin and put the tooth on the pin already. So, everything went just fine, they gave an injection, and it wasn’t painful to put an injection (after the second needle puncture, nothing is felt at all), and the first two punctures barely nibbled. They removed the nerve, inserted the pin, increased, that's all. By the way, I was afraid to go to the dentist hysterically, the consequences of dental treatment in the USSR affected. Now medicine has stepped far, now I'm not afraid to treat my teeth)
Yeah, she stepped so stepped! To cure or replace all teeth is the floor of the machine! In the USSR, at least everything was free. And the pain can be tolerated, then there was also freezing. And do not drag on a happy time in the history of Russia.
Removal after anesthesia was easy. But when I removed the nerve, I bounced in the chair, 3 injections did not work. Put arsenic. My tooth hurts.
Now it is a very strong painkiller, it does not hurt at all.
Now I'm treating my teeth in the district clinic. What should I do, advise? Many drugs do not affect my body. On 7 tooth, lidocaine injections were made several times. Three times put a temporary seal with the medicine. Just now they removed the last nerve. Here again with a temporary seal until the 15th. But other teeth are in poor condition. Also, the nerve must be removed. What anesthesia really soothes the dental nerve so it doesn’t hurt to remove ?! Here's a joke. Lidocaine is put and the tooth is removed. No sensations, even a cyst was scraped. And a nerve from a tooth cannot be reassured. Almost throws out of a chair.
So lidocaine is not considered the most powerful. Of the most popular - ultracain. According to the chain from the USSR: novocaine, lidocaine, ultracaine. But I agree, even ultarkain sometimes does not take particularly sensitive ones.
This is my problem. During the operation, the nervous system was affected in his youth. Now the nerves to hell. On the one hand, the reaction is excellent. On the other hand, the nervous system is very sensitive.
Hello, Alexey! You yourself write that you are treating your teeth in the district clinic, and according to the protocol, it officially takes time no more than 20 minutes per patient. During this time, the doctor should anesthetize and treat the canals, although in fact the treatment of the canals should not take less than 40 minutes, hours or more. If you can’t be offered import anesthesia as opposed to the free, not always effective Lidocaine, this complements the same arguments that are given above. If the clinic does not have modern anesthetics, then you should choose another institution where the emphasis is not on the “RECEPTION” of the patient, but on the end result - a painless and high-quality treatment of the tooth canals with subsequent filling (restoration with “filling”).
As for the arguments about the painlessness of the removal of the same Lidocaine.The fact is that this once again confirms that you can be “frozen” well, only the technique (and the anesthetic itself) needs an individual one for you. In a budgetary institution, everything is under the “RECEPTION” standard: there are a lot of people, and a HOSPITAL is a hospital, and a doctor is a doctor. The only thing you risk now is to get a negative impression, refuse treatment altogether and lose your tooth in a short time. Be healthy and receive only professional dental treatment!
I agree with you on everything! In 1998, they did all my teeth in an elite private clinic. One tooth cost 500-650 rubles (after a devaluation of 1000). Then there was money. Now, for a wheelchair pension of 4,037 rubles, try to do something! One heating costs 2450 rubles already. in kopeck piece.
Where is everything going? Peers die out like flies.
I apologize. Moved away from the topic. So, on the topic. Then they made fillings with a guarantee for 10 years. They lasted for almost 15 of me (some are still normal). Then, of course, one after another they began to fly out. That light-curing, it goes without saying, but ... Then they talked about the 5-6th generation and gel fillings. Now I’m telling the doctors, they pretend that they are hearing about such people for the first time. Warranty year. Also light curing, but 2-3.
And according to the insurance policy, only cement, which I personally have never kept for more than a month, is free of charge in the district clinic. Therefore, all the teeth from childhood and exuded. Of course, you need to put a good light curing. Her adherence is several times better.
Try ultracain.
Alexei, go to the paid one, there they will do everything painlessly. They even removed my nerve, and then - in general, not a bit of pain was there, it’s just unpleasant, that's all!
A similar situation. It turns out I'm not such a phenomenon (
Ubistesin + lidocaine.
Ubistesin is a powerful drug.
I am 13 years old. Today I went to fill the tooth, the doctor told me that in a week I’ll have to remove the nerve and then fill the tooth. Very scary.
Same thing, I'm 13 years old too. But only they will do it at school for the first time. I sat on the dentist's chair. They put arsenic 2 times, and on Tuesday or Wednesday they will get a nerve, I'm afraid. They say that Corvalol needs to be drunk an hour before the doctor. Or just ask for an injection to be done. But still somehow scary!
I have the same.
On Monday, I need to remove the nerve on the 6th upper tooth. I'm scared. Some write that with anesthesia it hurts. Is it true? Help!
Hello, Anya! “Some” is a small percentage of statistics. In a normal clinic, a professional doctor the statistics of such cases does not exceed 1% per month. And even then, most often it’s not pain, but soreness after the removal of the “nerve” in the process of passage of the channels.
Most often, the statistics on pain during the treatment of tooth canals are associated with budget (free) dentistry, when either weak preparations are used or the specialists themselves are “weak” in relation to knowledge of the correct technique for anesthetizing the teeth in the upper and lower jaw. I think your fears at the moment are similar in some ways to the purchase of household appliances (if the store does not have a check): is the fear of buying an inoperative TV or refrigerator justified? In theory, such a probability exists, but you cannot know in advance whether you will fall into that insignificant percentage of unlucky buyers or not.
However, you can always go to the store that friends recommended, where there are guarantees, a solid service and equipment are always good, and the brand is proven, especially where it will be checked and reassured.Then there will be much less fears.
I think that you understand my analogy, take a deep breath and try to find more reasons for optimism. If only because your tooth, thank God, is not the lower sixth, but for the lower 6 and “freezing” it is somewhat unusual and difficult in terms of the stability of pain relief. The upper 6 teeth with an imported anesthetic almost always “freeze” 100% well.
And it was necessary for you, doctor, to mention precisely the lower “six”. I have to depulpate just her. I can’t even sleep from fear, I’m odontophobe, which ones to look for, and here you are with your clarification. And where do I get optimism now?
No, it doesn’t hurt!
I am 13 years old, they removed my nerve with anesthesia, it does not hurt. You lie and everything is fine)) Only after the nerve is killed will the tooth be very sick. I personally now have the 7th day now ...
Today I went to the dentist, treated the front tooth on top of the second tooth. There was a small hole, and when the doctor drilled - it turned out that tooth decay damaged the entire tooth from the inside. The doctor cleaned, put a permanent seal, and two hours later an unbearable pain began. I called the doctor at the hospital, he said that I went to remove the nerve. Why didn't he do it right away?
Hello Light! I think that your purely human message is to accuse the doctor of the fact that he "did not immediately remove the nerve." I'm afraid that not everything is so simple. If we are talking about a public institution, then everything is more or less clear: most often a doctor is limited in time, and it is much easier to try to do something in one visit than to stretch it into several (this is about pulpitis). As for the fact that there was a small “caries” in the tooth, and the doctor turned it into a big one: in fact, the doctor did the right thing here that he processed the carious tissues in the volume that was not really hackneyed. Believe me, it’s not a pleasure for any doctor (even a private trader) to raise water-air dust from your oral cavity for a long time towards your dressing gown, hands, face, hair, etc.
Often, pain after filling is caused by a violation of technical nuances: the tooth warmed up during processing, as there was little water, the tip vibration was large, the “nerve” was close, etc.
I think that it makes no sense to clarify your last question in the context of the fact that you still will not find at what point the doctor could not have overlooked or made a mistake. But I can say that, by analogy with your question, they often ask me something like: “Tell me, please, I had a small hole in my tooth, and for some reason the doctor opened up his whole tooth and pulled out all the nerves, why did he specially make the tooth dead Was it possible to leave him alive? ”
Thus, how many clinical cases - so many opinions. It’s extremely difficult to please everyone!
I treated 4 teeth in one visit, put 2 pins, put teeth under the crowns on them, removed the roots and filled the tooth. AND EVERYTHING IS NOT HURT! True, she paid ten thousand for everything, they did an X-ray there right away, but I do not regret the money, I would have run away in the municipality in the first minute, and then I sat quietly for almost four hours. Thanks to my doctor, Marina Nikolaevna!
Good afternoon, Lydia! Tell me, please, in which clinic did you treat?
Daughters 16 years old, a dentist said today that she needed to remove a nerve, they thought that there was a small caries, and when they opened the hole, there was a huge hole.
If the nerve is removed, how long will this “dead tooth" live?
Hello, Lena! The question is extremely interesting and too subjective. I’ll try to express my point of view, based on almost 10 years of experience as a dentist, as well as logic and common sense.Let’s turn the question a bit and ask it like this: “And if the nerve is not removed, how long will the diseased tooth live?” I think that the answer is obvious: life is not comfortable, infection in the channels, the risks of receiving flux for the entire facade at any given time are great (in particular, on holidays or weekends). We can say that here from pulpitis to tooth extraction is one step, but the tooth is permanent.
Now back to the essence of the question: your daughter was determined by the doctor "pulpitis", the carious cavity has progressed for a long time, but in a hidden form. Of course, one can doubt that the doctor purely theoretically converted deep caries into pulpitis in order to treat the canals for his own pleasure, but here, you know, you can’t add my opinion to anything: you didn’t stand behind the doctor, he didn’t hold his hand.
Regarding the life of “dead” teeth, it’s hard to say for sure: the process of decaying of teeth without pulp is the result of many factors. I can only list the main ones: the volume of tooth tissues lost, occlusal features, filling height, nutritional nature, group affiliation of the tooth, filling technique, etc. If more than 50% of the tooth is lost, the tooth is chewing; if it is, it “holds the bite,” the child likes to gnaw pens, bones, acorns, etc., the doctor put the filling quickly, in thick layers, incorrectly shaded the filling, left thin tooth walls, edges, God forbid, carious tissues, etc., sometimes 1 of these factors is enough to “break off a dead” tooth in the next couple of weeks or months. Therefore, at present, there is a protocol for preserving a "dead" tooth, not with an ordinary filling, but with a tab + crown. Almost all of my patients on such an offer simply twist a finger at the temple. Indeed, why pay so much money to make a stump tab instead of a seal on a tooth, and already close it with a crown?
And here we return to what is written above: in this case, the life of a "dead" tooth is almost 100% extended to significant figures (from 8-10 years to 20-25). This technique allows him to be protected as much as possible from various surprises, starting from the doctor’s mistakes in the difficult restoration of the tooth with a filling and ending with protection against unauthorized loads on the tooth. The insert and crown are orthopedic constructions that are manufactured exactly according to the cast, minimizing errors in the details.
However, each person chooses what is best for him "for the money", but listening to the advice of a doctor. If the tooth is damaged by more than 50%, then it is advisable to think about its safety for years. In other cases, this is a personal matter for each person, but be aware that a priori “dead” tooth becomes more and more fragile over the years.
My “dead tooth” lived for 18 years with a seal, then it broke. Now I will make a crown with a tab.
Today sawed teeth for cermet. Everyone told me that it doesn’t hurt, but is slightly uncomfortable. Apparently, my dentist used to work as a butcher before ... Desna tore into “ribbons”. The process was periodically anesthetized with a spray, there was blood. I tried to moo from pain, but in a sharp form it was said: "You are straining me." I did not know that by “cutting a tooth” is meant “cutting a gum” ... I am terrified. After all, casts have already been taken.
I watched now a video about removing a nerve from a tooth: / And a miracle happened! My tooth, which was sick for 5 days (painkillers no longer helped), stopped hurting! Apparently from fear 🙂
Also just watched this video. The miracle did not spread to me ((
Yesterday I removed a nerve in my front teeth and put a seal. After the anesthesia subsided, a temperature of 38.3 appeared, 37.5 fell, and again, when biting, a slight pain is felt.
How to remove a nerve? Painfully?
They will remove my nerve tomorrow. Fearfully!
Me too
10 years ago they removed the nerve on the lower six, it was horror, I thought I would die from pain. And so, in principle, they did well, only recently I updated the seal. Now the top six is worried, a year ago it renewed the filling on it, after that, on the cheek side there was a sensitivity to cold and hot, and rarely there is not a strong throbbing pain inside. After going to the dentist, they treated this tooth with fluoride varnish (I don’t remember the name), they said that if it would bother me anyway, then they would most likely remove the nerve. Sensitivity is not completely, but passed. Or is it better not to delay nerve removal?
Hello! If you had a place to have spontaneous throbbing pain in the tooth or for a long time not passing, then we are talking about pulpitis or periodontitis. That is, it is necessary to treat the tooth canals with their subsequent filling. However, if your sensitivity appeared for a short time and only from irritants, then it is worth making an EDI of the tooth, before starting treatment of the canals. If according to the device’s data it is worth treating the canals, then it is recommended to do this immediately. If the pulp is healthy in the instrument, then you can follow the doctor’s instructions: in extreme cases, simply replace the seal with a new, more tight one.
Without the indications of the device, treatment can take place purely on a hunch: it will hurt - it will not hurt. Not all clinics have EDI, so you have a difficult choice. I can say approximately that 70-80% percent, you probably have to treat the channels, as there are certain suspicions of pulpitis. Would you submit a tooth picture for analysis?
I have a panoramic shot of the teeth. Do you drop it here?
Yes, you can here. For example, as a link to a file located on Yandex-Disk.
Hello! After analyzing the image, I’ll say that at the top of the root of the tooth treated many years ago there is a granuloma or cyst. And a decent size. Definitely this tooth may have an aggravation. As for the upper teeth: either 5 or 6 has a hidden carious cavity. It’s not exactly visible - this must be further analyzed already at the reception. But the picture well illustrates the tragedy in the lower treated tooth, where the distant canal is poorly sealed - hence the grown granuloma. Go to the dentist urgently, and the upper tooth will still have to be found in the mouth, and the picture will be an indirect assistant.
Hello! Thank you for your help, I will treat.
(The picture is attached, the link is available only to the doctor ...)
Hello! My name is Diana and I am 15 years old. Today I was at the dentist, checked my teeth. It turned out that I have one tooth (the fourth from above) is completely destroyed, they said to remove the nerve. I am very afraid that they never removed a nerve from my tooth, this whole thing came to tears. As a result, enrolled in a paid clinic on Wednesday. Actually, why am I writing all this, I would like to ask you if it hurts?
Hello, Diana! Many factors can affect the effectiveness of anesthesia, but more often than 80% of its level depends on the hands of the doctor. There is good news: this is the upper tooth and the fourth (as I understand it, you spelled the number correctly, that is, is it the one that goes right after the canine?), So it’s easier to make anesthesia without errors.
The only thing is that the 4 upper tooth is a two-channel one, but this is not a serious obstacle to a successful treatment. Stress affects the effectiveness of anesthesia, but rarely. However, it is worthwhile to calm down so as not to interfere with the doctor's work. No professional doctor is specially inclined to hurt you. Imported anesthetics are now working wonders.
In my practice, cases of repeated injections of anesthesia in the treatment of 4 upper teeth are extremely rare. I think that even with force majeure, the doctor will re-introduce the imported anesthetic drug and everything will be fine. In general, the treatment of tooth canals is an ordinary manipulation. Sometimes in some shifts it is necessary to treat the canals more than caries. With the help of canal treatment, the tooth is saved from removal - this is worth remembering. Even if the risk that “freezing” will affect 40-50% is about 1-2%, this does not mean that you should sit at home and wait for the tooth to “rot”. Since you have a 100% chance of a painless treatment by the group affiliation (and the fact that the upper one), I’m even happy for you with something: specifically because you don’t start your experience of treating tooth canals with the lower big molar tooth. Lower molars are more prone to the vagaries of anesthesia, especially in the inexperienced hands of dentists.
Many thanks!
Dear Patients! Come for an inspection every 6 months. And you are cheaper and easier for us.
Cynically! But for sure, unfortunately ...
Hello! I am 33 years old, finally decided to put braces on my crooked teeth, stopped with an orthodontist on metal. 3 months wore, everything was in order. After the next change of the arc, after about a week, there was just a hell of a pain in temperature: from hot and cold there was a sharp pain in the jaw above the canine, but not constant, only during meals, if the food was not at room temperature, and a few minutes after ... First I couldn’t understand what kind of pain, I thought that because of the braces, after the change of arc, they had not yet “moved away”. But then I realized that the nerve of some upper tooth hurts. Later, she found a small seal in the area of the canine root - it hurt! All this charm fell on the holidays, and did not immediately run to the doctor. And after a couple of days the pain began to subside and then it appeared only from the cold, and if you quickly drink it with, say, warm water, then it “let go”. I went to the doctor. The orthodontist said that, most likely, pulpitis, it is necessary to take a picture and to the therapist. The picture was taken: besides the teeth “moving”, the picture showed nothing. The therapist said that the picture "should not hurt anything."
Nevertheless, the orthodontist removed the arc after me, after it was treated with fluoride varnish and told to wait, while everyone felt the same seal, the “ball” on the root of the canine. There is no caries, as I understood, none of the doctors wanted to remove my nerve without acute pain. I think that this ball is an abscess that sits there ... It turns out. what do I have to wait for it to break through, I will die of pain, and only then will my nerve be removed? Or this abscess (if it is), or a seal, can itself go away? It reacts to the cold gum above the canine, plus I feel the air, there are painful sensations if you press on the face at the junction of the nose and nasolabies. Absolutely, it’s not a tooth, it was tapped and checked with air, it seems that the seal hurts. Why doctors do not want to remove the nerve?
Hello! The version of the "abscess" is excluded. The fact is that only a “living” tooth in which there is a full-fledged “nerve” can react to cold. Of course, this does not mean that the “nerve” cannot be affected by the inflammatory process, but while the tooth reacts to the cold, it is too early to speak of “abscesses” at the root. Since you have fast-passing pains only from external stimuli, even caries or increased sensitivity of enamel can be assumed. The mystery of the resulting compaction against the background of orthodontic treatment suggests that the canine is excessively “displaced”, and this somehow affects the basal area of the canine.
Of course, all this is speculation. The fact that this is not an "abscess", so far - 100%. Another question: it is most difficult to understand against the background of what the problem arose. Obviously, doctors either feel sorry for working with a fang, or do not really want to.The best moment of diagnosis could be EDI - electroodontodiagnosis. That is, a measurement using a pulp excitability device. If the pulp is healthy, then there may be latent caries on the canine or increased sensitivity. And against the background of whether orthodontic treatment this sensitivity has appeared - it will be difficult to say anyway.
If the device shows that the excitability is reduced, then the pulp should be "removed" from the channel 100%. Here, not a single doctor will be screwed up. However, the difficulty is that this device is not available in all clinics. I would say: most clinics somehow ignore it and do without EDI. In your case, such a diagnosis would answer half the questions.
Thanks a lot for the answer and for the advice! The fact that there is no abscess, you are absolutely right, because every day I feel better, the pain has disappeared completely, I can even eat ice cream, the condensation is still painful and pressing on it ... Regarding the fact that the fang began to shift too quickly, You, too, are absolutely right, I also thought about this, all the more so, from the very beginning he very much “stuck forward” and very quickly got in a row. Now, apparently, there is no need to wear an arc on the upper jaw yet and I will look for EDI!
They opened my tooth and removed the nerve and told me to come rinse. But how to rinse, does it hurt?
Hello, Anya! Some stupidity - I’ll say right away. With pulpitis, the canal is washed immediately with subsequent filling of the canal with the modern method. There are treatment options with staging with gangrenous pulpitis of an antiseptic dressing in the canals, but then it is simply removed for the next visit, repeated treatment is carried out with the same tool and filling (without it, nowhere).
I think that you are being treated for purulent periodontitis, in which there could be no “nerve” a priori, since it decomposed for obvious reasons. If you are being treated with the open canal method, then this method is too routine: many dentists criticize it for the risk of re-infection of the canal from the oral cavity. As for pain with such treatment, this is a question of the principle of the method. It is solved individually; preliminary anesthesia is often used.
They want to remove my dental nerve soon. I am 14 years old, this is my first time, the procedure costs 3600 rubles, will it hurt? Tell me please.
Hello Walihan! Information is not enough for me to throw off approximate statistics. I will explain why. The most important thing is the group affiliation of the tooth and the qualifications (experience) of the dentist. There are teeth that any practicing dentist can “freeze”. However, for example, at your age, for a number of doctors, a problem can be a painless treatment of the lower large molars: the sixth and seventh. Of course, the younger the age, the more difficult it is for most dentists to get quality anesthesia. However, experienced dentists know a lot of tricks to achieve persistent anesthesia in this age group for the treatment of any tooth.
That is why, I can’t tell you with 100% accuracy: it will hurt or not. Another question is that, most likely, about 70-80% of cases pass painlessly in private clinics. Unlike state (free) dentistry, where the doctor takes patients quickly and not always with high quality. I am sure that the doctor will do everything possible so that it does not hurt. Modern anesthetics allow for absolutely painless procedures in dentistry. So hope for the best and trust an experienced doctor! Good luck
Thanks a lot.
The tooth aches after the expansion of the tooth canals, a permanent filling will be delivered after 2 days. I know that it’s normal when a tooth hurts, but how to get rid of pain anyway?
Hello! Unfortunately, prescribing drugs in absentia is prohibited. The fact is that, as an example, you may be allergic to certain drugs. The best option is to analyze the image after filling the canals, and then draw conclusions about how to use home remedies to relieve post-filling pains.
It's okay, it makes no sense to be afraid.
Hello today, they put in arsenic, they said to come in a week to remove it. Is it not a long time to walk with him, or rather, is it not dangerous? Then remove the nerve, very afraid it does not hurt? And can I ask the doctor for anesthesia?
Hello! Arsenic paste - an old technique, it is better to at least be non-arsenic analogues. However, if you have already begun to be treated in this way, then it is worth clarifying: did you put the arsenic exactly, maybe you did not understand the doctor? Arsenic paste is placed for a maximum of 48 hours (2 days), and arsenic-free paste - up to 5-7 days or more (travel option).
I always carry out treatment with anesthesia, I think that the doctor will definitely do it, but it's worth asking, just in case. Have a good treatment!
Today I was at the dentist, I drilled a chewing tooth, said that it was necessary to remove the nerves, to fill 3 channels and put a permanent filling. All this costs 7000. Normal price? Since there was no such money with me, I put a temporary seal with arsenic.
Hello! The norm is that of the majority. From the point of view of pricing policy - this is a normal price, for megacities - even below average. Another question, what do you offer for this price? I’ll explain approximately: canal treatment is the most expensive pleasure at this final price, since it is labor-intensive, difficult, responsible and in every sense energy and materially expensive.
That is why the clinic summarizes the list of procedures that are included in the treatment of canals: expanding, passing, washing with such and such, applying ultrasound and / or a microscope during their processing, filling the channels with lateral condensation of gutta-percha, hot gutta-percha, Termafil, etc., images (diagnostic, control, temporary filling, etc.) The average price for treating canals (6 or 7 teeth) under a microscope is about 15-20 thousand rubles per treatment: canals + light-cured filling ( e.g. Filtek or Grady a).
The patient pays not only for specific microservices during canal treatment and tooth fillings, but for the level of equipment of the clinic and the professionalism of the dentist. If for 7 thousand rubles this symbiosis of all of the above corresponds to quality and a guarantee for treatment (usually about a year for filling and more than 3-5 years for channels), then the price is adequate. In the meantime, I can say in absentia that this price is normal.
Yesterday I went to the dentist, and according to the results of the examination, it was recommended to remove the nerves of 6 from the bottom left. Since I am insured by VHI from working with a very impressive coverage in terms of dentistry, everything, absolutely all procedures, are free for me. So, after 3 injections with the most modern drug, the doctor began to drill ... At first everything was, it seemed, painless! But then the doctor got on my nerve and I started to twitch! They made another injection, already in the nerve, but it did not help. Only after 5-6 additional injections into the nerve did I stop feeling pain. Otherwise, everything was as described in the article.
Hello, I wanted to ask: if caries didn’t get to the nerves, and the doctor put a seal without removing the nerve, what will happen, then the tooth will hurt then?
Hello! The question is provocative and requires a long explanation. Most of this answer is an overly professional topic, so I will limit myself to a short explanation.If caries did not cause an inflammatory process in the pulp of the tooth, then a filling can be immediately put. When a non-professional takes on this matter, mistakes can lead to the fact that a carious tooth with a healthy pulp turns into pulpitis after treatment, that is, with a filling, such a tooth will begin to hurt, although it should not, in theory. If the doctor initially (before treatment) does not determine inflammation in the "nerve", then the effect will be the same - lack of success after filling.
If the diagnosis of "caries" is made correctly, and the doctor performed his manipulations without errors, then under the seal the tooth will not get sick. There are still some nuances: often the doctor, having made the correct diagnosis of "caries", makes a number of small mistakes during the work with light fillings, and you get pain when you click on the fillings or unpleasant sensations from cold (less often - hot). It is important to correctly assess the situation: if the pulp remains healthy, and the tooth hurts from irritants (especially when pressure is applied to it), then we are talking about the illiterate placement of the filling (especially with impaired preparation for the filling). A number of doctors suggest waiting until 2-3 weeks until the dentin recovers itself and stops testing the person, while other dentists recommend replacing the seal, but comply with all prescriptions according to the technology.
In general, Kaliza, the answer to your question is this: the tooth will not hurt if the diagnosis of caries is correctly made initially and when the treatment technology is followed - from preparation for the filling to its final polishing.
They will remove the nerve on my lower tooth, the first on the right, is it scary? And how is this process going?
Hello! If you say “first lower right”, you mean the lower incisor, then 100% you can not worry, since these teeth are not difficult to anesthetize. In this tooth there are both one and two channels, the "nerve" under anesthesia is removed without pain. If, however, “first on the right,” you mean a 7 or 8 tooth (the eighth is a wisdom tooth), then I can assume that in about 70-80% of cases everything will go fine. The fact is that it’s technically difficult to freeze such teeth, but this is not difficult for experienced specialists, since from the theoretical and practical side they are well-versed and know all the possibilities of qualitatively anesthetizing 7 and 8 teeth. In the 7 lower teeth, most often there are three channels, in the eighth it happens arbitrarily, but most often the lower wisdom teeth, unlike the upper wise teeth, are not so complicated, and somewhere even easier - 3-4 channels are treated.
Treatment of tooth canals begins with anesthesia, then the tooth is prepared, access to the mouth (mouths) of the canals is opened, thin “needles” (files) are inserted into the canal, which pass the canals along the entire length, and then expand under the filling material for the canals. Most often, they fill with paste + gutta-percha pins. They tightly stuff the canals, and then adjust and put a temporary seal until the next visit. At the end, a filling is placed already on the upper (crown) part of the tooth. In principle, not scary, but responsible: on the part of the doctor and patient.
Thanks.
The third time they put a temporary filling on arsenic, maybe they poorly cover it and the nerve is not killed? Could this be?
Hello! Unfortunately, I had previously encountered such a problem myself: I haven’t been working with arsenic pastes for many years, but have been using non-arsenic pastes, but the point is the same. Honestly, in 95% of cases this is a lack of knowledge and experience of high-quality anesthesia, because many dentists generally work without drugs for nerve devitalization - they immediately treat the channels of any tooth, and devitalizing paste is used only 3-5 times a year in the most difficult situations. At the children's reception, one can still assume some individual characteristics of the tooth and the structure of the jaw, but in adults it is much simpler.Therefore, if your case does not apply to 5% of the options associated with the obstacles of anesthesia (drugs, alcohol, strong fear, etc.), then the doctor does not use all the possibilities of imported anesthesia.
As for the second problem you voiced (arsenic does not work, as you call it), this happens when:
1. Incorrect paste;
2. Too wide and long channels with massive pulp with insufficient amount of funds.
However, I emphasize once again that in most cases, paste for devitalization and pulp is a dentist reinsurance and no more. Let them focus on the quality of the anesthetic and the technique of anesthesia!
After improper removal of the nerve (the doctor could not find for a long time), everything around was inflamed. Two months from the gums were spotting, swelling. The teeth parted, the gum does not stick to the teeth. Now I took a picture. They said the channel is sealed well. But this is already chronic. Or endure, or remove a tooth. Very sorry. Advise what to do?
Hello, Lyudmila! If you describe everything correctly, then you suffer from an exacerbation of chronic periodontitis: it is possible that there is a perforation of the root or bottom of the tooth, due to which there is a moment of evacuation of bloody and (or) purulent exudate through the marginal gum. As for the fact that “the channels are sealed well,” I can only advise you to check this seal by providing a snapshot - either here (via mail, or as a link), or from an independent expert in the chair. This cannot be so that for no reason the gums are “swollen”. Not knowing your age and features of the gingival attachment, it is difficult for me to suggest or refute periodontitis. Periodontitis is a problem that is not related in this context to the treatment of canals. Coincidence - not a coincidence? Again, I return to the need to see at least a picture with my own eyes, and then it will become clear: is it necessary to have a dental examination and detailed diagnostics (probing, percussion, palpation of the gums, determination of tooth mobility), or will the verdict already be 100% - tooth extraction dental surgeon. So I advise you to get a picture and (or) immediately from an independent dentist in a chair look around and understand the reason. I wish you a speedy solution to the problem!
Good afternoon! Was at the dentist 5 years ago. Put a seal. After 2 years, it fell out. Recently I decided to go again, on the lower tooth we renewed the seal 10 years ago, but on the account of where the seal fell, said pulpitis. The top 5 or 6 on the left - said, will remove the nerve and seal. I asked how many visits there will be, the doctor said - one thing. Question: will it be right to immediately remove the nerve and close the seal in one visit?
Hello Anastasia! The question is just wonderful. For many years I have been watching how many dentists (about 30-40%) are treating canals and filling a filling in one visit, motivating me that in one visit it saves time with the same results. Personally, I do not put it at a time, because I see no reason to put a light seal on the uncured material in the channel with or without a gasket. Many doctors agree with me, and an example for me is a professor of therapeutic dentistry (a doctor of the highest category), who prefers to carry out temporary tooth restoration after canal treatment. What does this mean: canals are sealed in a modern way to physiological constriction, controlled by a picture and sealed (top) with some cheap “permanent” material, which gives excellent tightness to the tooth, but it involves replacing this, all the same, temporary material with high-quality constant light-cured seal or restoration.
The whole “fuss” due to the fact that the material shrinks in the channels of the tooth over the past few days, and the tightness of the permanent filling may be impaired (microcracks and “leaks” occur). This can be ruled out by the permutation of a temporary filling to a permanent one 3-5 days after endodontic treatment.
Thank you for your reply! Health to you and your patients!
Hello, tell me, and when does caries reach the pulp and constant aching pains begin, then if not treated, how long will they last? I had a toothache a year or 2 ago (somewhere around the top fifth), for 2 or 3 days, ached constantly and very badly. It seems like it looks like pulpitis, but then it somehow suddenly stopped hurting, even reacts to sweets, although, as I understand it, this only happens with live pulp. What could it be?
I forgot to add that now the tooth does not bother at all almost only if there is any chocolate to eat. It does not respond to hot, cold, pressure, etc. (but there is caries).
Hello! If you want not to treat your teeth, but try to find an explanation for this possibility, then this is a dead end, but your business. Well, firstly, the pulp does not always die in a short time without treatment (from 2-3 days to 3-5 months), but most often (in 90-95%).
Secondly, the tooth that you ached (pulpitis) could stop hurting due to the compensation of the body and the protective reaction of the pulp from infection, but the adjacent tooth has a commonplace caries. I often encounter such cases: next to a dead tooth (periodontitis) is absolutely alive, but with average caries and reacts to sweets. So, based on your practice, you either have a dead tooth decayed by caries before the pulp chamber and a carious neighboring living tooth, or a chronic pulpitis that is still chronic, but caries on the neighboring tooth also, as in the first case, gives a reaction to sweets.
Chronic pulpitis, as well as some forms of periodontitis, may not be asymptomatic for years in all people, but the process of even asymptomatic tooth decay is a risk of serious complications and tooth loss due to their transformation into “roots”. Often this can be heard at the reception: “At first the tooth was very sick, then it stopped reacting for many years, and then it broke off yesterday and the root started to hurt, the cheek was swollen, you couldn’t touch it, it would be better to heal right away, and now you have no teeth - only remove residues. "
Hello, Svyatoslav Gennadievich ... Tell me, please, today the last tooth fell, the lower right (the so-called wisdom tooth). Next to him pulpitis was treated in a free clinic. Many channels were very painful. Tell me, what problems will be with this last tooth? Thanks in advance.
Forgot to report. The tooth hurts, but you can eat. The tooth is whole, without holes. What could it be? As if the gums were slightly swollen, where the teeth were gone. Beyond this tooth.
Hello Igor! Without examining the oral cavity, it is difficult to unequivocally judge, but judging by the description, you have a difficult teething wisdom tooth (pericoronitis). If the edge of the wisdom tooth is slightly covered with a “hood” of the gum, then there is a high risk of pain due to the tooth trying to break through the thickness of the tissue. The infectious component also affects: with incomplete eruption of the tooth, there may be a throw of food into the space between the tooth and the gum, which provokes inflammation. In any case, this is an occasion to contact the dentist for confirmation of the diagnosis and decision regarding the wisdom tooth. The verdict depends on the individual tactics of the doctor in this clinical situation. If in the future there are serious risks of repetitions (relapses), or a more serious infectious inflammatory process, then the eighth tooth is removed. However, a number of dentists prefer to help the tooth with excision of the “hood”.This practice is not welcomed by all doctors, as it sometimes leads to new phenomena of pericoronitis, or to its complications (extremely rare). Of course, only your doctor should decide here.
As for the penultimate tooth previously treated: if you doubt the correct treatment of its canals, you can take a diagnostic picture and provide it via mail or as a link. The only thing that according to the description is it is important to first eliminate pericoronitis in time, and then deal with the possible problems of the 7th tooth in the distant future. Good luck
16 years ago I faced just such a problem. The wisdom tooth did not fully crawl out. An inflammation has formed under the hood. The dentist cut the gum. After some time, the gums grew again and inflammation started. I got an appointment with another doctor. She rejected the colleague’s offer to remove the tooth, arguing that there is an antagonist and that she will always have time to pull out. I cut the gums, burnt. She gave her phone number and said that if she repeats herself, call her and she will remove the tooth for free.
Very grateful to this doctor. The tooth is still intact (although the antagonist was lost several years ago) and no problems were created with it anymore. Here would be more such professionals in free and paid clinics!
Tomorrow they will remove the nerve on the bottom 8, scary. Does it hurt or how?
Hello! It all depends on the professionalism of the dentist, the selected anesthetic and your mood. The latter is a must, as a positive attitude often works wonders. If the doctor does everything right, and you will be shaken from fear, and you will begin to listen to "your" feelings to the point of insanity, then the procedure can be painful. Stress affects the onset of quality anesthesia, I know from my own experience and the work of colleagues that it is often necessary to leave a patient with anesthesia for 15-20 minutes (under the supervision of a nurse) to enable him to let go of the situation, take a breath and not focus on his fears . I don’t think it’s normal to put a patient in the corridor for the same time in the hospital, but after that in many cases persistent anesthesia and treatment of the tooth canals are painless. A good nurse in the office can tell a joke, ask about the weather, cars, advise something, etc., in general, put nervous tension in a different direction. So do not be afraid and trust the experience and professionalism of doctors, well, and do not forget to remind the doctor that you prefer an “import” anesthetic against Lidocaine, and even less so, Novocaine. Good luck tomorrow!
Good afternoon! In the event of an injury, she broke 3 front teeth (2.1 to 1/2 of the height was broken, 1.1 and 2.2 - partial chips). Tooth 2.1 was depulped, the canal was filled 5 days ago. Further, the dentist recommends adding this tooth to the pin. 1.1. and 2.2 are extended, they don’t particularly bother, there is a slight discomfort with pressure and a slight “aching” pain periodically occurs. The dentist says that you may need to depulp and 2 other teeth. How necessary is it in my case?
Hello! The most accurate information (objective) is given by the EDI of the tooth. Not all clinics have a corresponding device. When determining the electrical excitability of the pulp, you can find out if there is an onset inflammatory process, or not. With injuries of this force, it is often necessary to have a tooth pulped. I don’t think that this is a big tragedy, since with a certain experience and professionalism of a doctor you can correct the imperfections of a smile, if that happens (bad teeth shape, slight bends, turns, unsatisfactory natural color of teeth, length of tooth crown, etc.) . That is, there are often even pluses from restoration, but the question, again, is whether to make the tooth “dead”?
If the pulp died by EDI, then without treatment of the canals, the tooth can be brought to periodontitis, periostitis and other purulent complications from which the face swells. If the pulp is healthy by EDI, then there is a chance to get by with the restoration without pins so far.
If the clinic does not have EDI, then you can compare your feelings with the diagnosis of pulpitis according to complaints. When the pain becomes spontaneous (without irritants), worse in the evening, at night and sometimes painkillers are required, then it is necessary to treat the canals - there is inflammation of the pulp. It doesn’t matter whether the pain is acute or aching. If the aching short painful reaction is only associated with the action of stimuli for some time (cold, hot, sweet, etc.), and without this the pain does not appear, then we can hope for dental treatment without removing the “nerve”. In any case, the last word is up to the attending physician, and you have the right to change the doctor if the position of the first does not suit you. Sometimes it is so necessary for controversial cases to hear the opinion of 2-3 colleagues in order to arrive at an unambiguous and maximally correct conclusion.
This consultation should not be considered a 2 opinion, since you can only outline an approximate plan in absentia, but I will not be able to fully examine the teeth and understand the scale of the problem. Thanks for the question.
Hello. I am 33 years old. A week ago, I turned to the dentist, there were no pains in the tooth, there was caries on the lower six. The tooth was drilled, caries removed. It was deep, as they said, did not reach the pulp, although at the end of the drilling procedure pain was felt. They put a temporary healing filling for 4 days. The tooth reacted to pressing and cold. The dentist said that the pain will pass after a permanent filling. I put a seal, light, and the tooth hurts also for 2 days. Even with light pressure on it, or cold water. It is impossible to eat on this side. Tell me, please, what to do next?
Hello! There is the most rational option - it is to find a clinic where they can conduct an EDI of a tooth - precisely and without cheating. If the pulp is in the stage of inflammation (even the initial one), then the device will show this, and it will be necessary to treat the channels. With a healthy pulp condition, it is advisable to re-fill the seal with a professional dentist. In this context, I do not think that the tooth is damaged, a number of technical nuances are simply violated, hence the sensitivity from the cold and when biting on the fillings.
The option to wait until 2-3 weeks is debatable, as there are certain risks that can lead (in case of pulp damage) to complications, although a number of dentists adhere to this approach.
Hello! My question is: there was a tooth filling, the second upper one from the end, chewing, in general. The doctor said, it is necessary to put a crown, first remove the nerves, clean the channels, put the stump. Are nerves removed right away or not?
Hello! Modern methods of treatment involve the treatment of canals in one visit: extraction of "nerves", passage, expansion of channels, drug treatment, filling for temporary restoration. The seal is most often put on the next visit. In your case, as I understand it, this is the tab on which the crown will then be “hooked”.
However, it is not a mistake to treat channels with the preliminary use of devitalizing paste (which kills the “nerve”). It is worth noting that arsenic paste is not favored in our time - it negatively affects periapical tissues and can provoke periodontitis in the future. Armless - you can set, but also added an extra visit and (often) uncomfortable or painful sensations while walking with her.
Therefore, simultaneous treatment of canals is the most preferable in our time, with the exception of special situations. Have a good treatment under the tab + crown.
Thank you very much for the answer!
Hello! I want to ask your advice. I’m 22, I recently had a seal that was placed in my school years, everything was black under it, and before that this tooth was problematic - a little overcooling, and it starts to itch inside or to throb. And this despite the fact that he is dead.
I went to a paid clinic in which I was already, whom I trust relatively. The dentist brushed my tooth, it turned out that the roots are in order, there is no blackness. But for the sake of order, they took a picture, and it turned out that in one of the channels of the tooth there is a residue of a metal tool with which they are cleaned. Plus, there is a slight round inflammation under this root. In the end, she said that she was not sure that she would be able to pull out the chip, so I had to decide whether to pick the channel or not. I was afraid.
And now it’s cold outside and the tooth periodically flips. The question is whether it is worth panicking and doing something, or if there is no danger of increased inflammation, then you can not worry? She closed her tooth in good conscience.
Hello! I think that you just left a "time bomb." Here it’s hard for me not to advise you to treat the tooth canal and eliminate the inflammatory process using an affordable method. You can try to remove the fragment using ultrasound equipment using a microscope, and then put in the channel a preparation based on calcium hydroxide for a period of 2-3 months to a year with periodic replacement of the material.
Otherwise, the inflammatory focus will exist in the stage of compensation until the next exacerbation: hypothermia, stress, general diseases, hormonal failure, etc. can lead to this. Therefore, if the dentist “patched up the tooth”, then we are talking about the upper (crown) part, which will not help the tooth in the long run absolutely. That is, the reason for excitement remains.
Thanks for the answer! Oh, you have to walk around with a time-bombed mine in your mouth until you have the opportunity to treat the tooth) It's a shame, however, apparently my dentist was not ready for this turn of events. It looks like you have to find another place for the tooth to be treated. I hope in my city there are dentists involved in this.
Hello! In mid-August, 3 nerves were removed from the top six, and pins were installed. After 1.5 weeks, the tooth began to respond to hot. Reacts to this day. I went again twice to my doctor, but he did not give a reason and did not say what to do. Tell me, please, why does a “dead” tooth react to a hot tooth and what should be done?
Hello! If this particular tooth creates such problems, then we are talking about defective processing and (or) defective filling of the channels. In the upper 6 tooth almost always (in more than 80% of cases) there is a 4th channel (according to the latest statistics). If even the 4th channel converges in the main one in the mesial buccal root, all the same, the void even in the narrow canal is abnormal. Just these symptoms are possible with a similar error. Other technical errors could also lead to an aggravation in the same form as yours.
I can advise only one thing: to examine the 6th tooth from the picture. If possible, then for analysis you can send pictures to the mail (see the "Feedback" section), I will tell you if there is a (approximately) problem. It all depends on the quality of the picture and the viewing angle. If anything is revealed, then 6 teeth will have to be treated. If the problem in this tooth is not confirmed, then it will be necessary to diagnose neighboring teeth, but all this is already in the dentist's chair. Thanks for the question.
Hello, my tooth was half crushed and it started to get dark inside, sometimes it hurts, but not very much. How is this dangerous? And what will the dentist do? I'm just terribly afraid to go to the doctor. The third tooth is from the bottom right.
Hello! According to such small data, it is difficult for me to predict the further situation, but it’s already certain that sooner or later this will lead to tooth loss. In what form it will be: simply removing the “calm”, but destroyed under the gum root, or you will need emergency help due to severe pain, high temperature, “flux”, etc. - not known.
I think that the dentist’s tactics will be as follows: analysis of the root canals and tissues beyond the borders of the image, after which treatment will be planned. Sometimes the doctor from the picture can offer immediate removal, but in your hands get advice from another 2-3 doctors in other clinics, where there are ways to save even the most complex teeth. The treatment plan will depend on the situation in the canal and outside the root. That is, treatment can end in one day, and can drag on for 2-3 or more receptions. The dentist can limit himself to just a filling, but can also start treating the canals. In any case, everything is done under local anesthesia. A professional will never create a situation where it will hurt you, since the most comfortable treatment for the patient is also beneficial for the doctor for a calm and full work. Do not be afraid and soon heal until it has "begun" ...
Hello! The fifth tooth from above began to feel hot and cold, sweet and sour, I think this is a pre-decay caries. Is it painful to treat it with ubistezin, and will the nerve be removed? There is no hole in the tooth, but there is only a slight damage to the enamel, sort of like, but this is definitely not a hole.
Hello! Based on your story, I think that you will receive cervical caries treatment without removing the “nerve”. Anesthesia is most often performed for patient comfort. The “nerve” is removed only as a last resort, especially since the placement of the seal will not interfere in the future (if the need arises) to process the channels, since access to the channels can only be obtained through the chewing surface. So you do not risk anything: a successful treatment for you!
I am 15 years old, went to the dentist today. There was a hole, I thought that you just need to put a seal and that's it. It turned out that it was necessary to remove the nerve. I was drilled a hole and put something, then they made a temporary seal, they told me to come next Monday. Will it hurt or not? 5 upper tooth.
Hello! I think that if you put the paste on the opened nerve with the treatment of the carious cavity, then this was done with anesthesia. Since you are not complaining about your first visit, then everything went well. This implies the fact that there is no point in fearing the second stage, because you transferred the living tooth to the dead, that is, you created all the conditions for its painless treatment. I will not criticize the treatment method using devitalizing pastes - it is, in principle, acceptable for budgetary forms of treatment. So good luck in the future, the main thing here is not to be afraid and trust the dentist!
Hello. On the sixth tooth, the filling was changed 3 weeks ago from the top. The doctor said that there was no pulpitis, protective dentin was developed, but had to be drilled deep enough. Now this tooth periodically aches. Does this mean that pulpitis has developed and still need to remove the nerve?
Hello! If spontaneous pain (that is, without an external irritant), especially confined to the evening (night) time, is worried, pulpitis has developed almost 100%, and the canals of the sixth tooth will have to be treated. Meanwhile, pain when biting on a tooth (filling) can indicate both pulpitis (periodontitis) and a post-filling reaction with a healthy pulp. Post-filling pain indicates violations during the placement of the seal and requires a technically correct re-installation of the seal.Ideally, EDI can provide accurate information, but only if your symptoms cannot tell your doctor if there is inflammation of the pulp or not (for example, if you are talking about soreness when biting on a tooth, pain from a cold, etc. ., but there are no obvious signs of pulpitis, about which I spoke above). The destruction of the pulp does not always occur with vivid clinical symptoms, therefore, there is an EDI to help the doctor - determining the electrical excitability of the pulp. If this device is not in the hospital, then everything is decided by the collected history and examination of the tooth in the oral cavity.
If in doubt, the pulp is usually removed and the canals are sealed, so to speak, without divining on the coffee grounds. Thanks for the question.
Good afternoon! I had a question, the situation is this: in childhood, they removed the bottom 6, and then grew 8. Both of the bottom 8 are functional (participate in the chewing process). In the 8th tooth, on the side where there is no 6th tooth, pulpitis. We decided not to delete because it is very, very needed))
At the moment, the channels are cleaned and the tooth is under a temporary filling with some antiseptic. It is necessary to choose what to close the tooth with a ceramic insert or seal. What could you advise?
The attending dentist says that control pictures will need to be done in a year to be sure that everything is in order with the tooth. And at this stage there are no guarantees that the tooth will not have to be removed in a year ((And I suggested the option - put the seal and remove it from the bite so that the upper tooth does not rest against it, and after a year put the tab.
And another question: 8 - the same teeth in strength as the rest? Or are they more fragile?
Hello! Firstly, it is difficult to judge without examination in the oral cavity how much this tooth is valuable and what are the prospects of its existence in the dentition for your benefit. Secondly, was there any pulpitis at all? Maybe the tooth is still being guided by the periodontitis diagnosis that is not quite convenient for the dentist? I am confused by the laying of antiseptic agents and a kind of “mouse fuss”: if we are talking about control images after a year, then it just falls under the monitoring of periodontitis at the stage of anti-inflammatory treatment, and for pulpitis (if you still talk about it) it’s too much and coupled with the wording “no guarantees that you don’t have to remove the tooth” and “you need to remove it from the bite”. Based on the data presented by you, I can say that the dentist either conducts periodontitis, or cannot qualitatively treat a given wisdom tooth (cannot pass channels along the length or does not find any channel, broke a tool, poorly sealed channels, created a false channel or made a perforation - many different factors sometimes push the dentist not to believe in the prospect of treatment).
As for the strength of 8 teeth: they are no different in this respect from the rest: if the tooth is badly damaged (more than 1/2), then, of course, there are risks that it will crumble in the future, since it is “dead”. Therefore, they offered you one of the most reliable options for restoring the crown part - a ceramic insert. In addition to the tab, the "dead" teeth are often still covered with a crown, which makes it possible to stand in the dentition for as long as possible. Only now, I doubt, starting from the words of your attending physician, that it is worth doing such an expensive job, saving the upper part of the tooth, when the dentist knows something about his inferior work (my assumption) inside the canals. If you send a picture with the treated channels, then perhaps I can give you a more complete analysis of its work.
A few days ago I was treating 2 front teeth (canine and tooth, which is next to it, to the center). The fang was in poor condition, but I only found out that I had to treat a tooth that was nearby, after examining a dentist. So, the fang nerve was not removed to me, and the 2nd tooth was removed.And now, after 4-5 days, I noticed that it had darkened. What is it connected with and will it pass over time?
Hello! I think that this itself will not work. The darkening is most likely due to the fact that the material used to stain the tooth was used, since a dead tooth in itself darkens gradually, or rather, it dims every year. Here we are obviously talking about some kind of external factor. Sometimes it happens that the staining is associated with bleeding from the canal, which was stopped with difficulty. Understand stands still - in the doctor’s chair. If you do not like the aesthetics of the tooth, you can use either endodontic whitening (usually this technique helps to improve the color characteristics of the tooth without losing its tissues and with the maximum positive effect), or restoration of the front wall of the tooth using light-cured material, making the so-called veneer a direct method. Thus, you will restore color and, as a result, aesthetics.
Today I went to the dentist and he said that I need to remove the nerve (from 16 teeth). I read the comments about the negligence of dentists - it was already scary. I wanted to ask, is it painful to remove the nerve?
Hello! To topulate the upper teeth is almost always painless. “Almost” - this means that there is practically no difficulty in technical terms to carry out painless removal of the “nerve”, but in rare cases, not quite an experienced dentist may not pay attention to anesthesia from the palate, and then the treatment can be a little painful. I think that you should choose an experienced dentist with at least 5 years of experience. Moreover, it is important to rely on the feedback of friends, acquaintances, relatives about this doctor (and come to the reception without fear and strong feelings, since the fear of tooth treatment sometimes prevents anesthesia from acting fully).
Hello) Panicky afraid to go to the dentist! Although I was not so afraid before. So, what I’m leading to: I was at the dentist’s, they put a seal on my front tooth, then, after two years, the tooth started to hurt. I went to the doctor again, he drilled a tooth behind me - there was a small hole (and I don’t know if they removed my nerve or not). The doctor told me two days later to come again, but I never came (which I regret very much now), and after a year somewhere the tooth broke under the root. Now I am very much afraid of what they will do to me, completely remove the root, or what? And will it hurt? Tell me please )
Hello! Nevertheless, the doctor removed the “nerve” for you, and a dead tooth, which has thin walls that the doctor did not have time to clean from caries and put in a seal, since you did not come to the second appointment, can break quite easily - which is what happened. Now it is important to evaluate the root for its suitability for further prosthetics of the tooth (that is, can the root be preserved at all). Here, you definitely need to contact the dentist for an appointment so that he evaluates the external characteristics of the root and takes a picture of it. If the doctor does not recommend preserving the tooth, it is important to have another 1-2 consultations with other doctors in order to form a general opinion that is close to objective. According to the picture, the dentist will assess the condition of the tissues surrounding the root for inflammation, since the tooth has been without a permanent filling for a long time. It is possible that root treatment is needed, but this is only for the good, so that in the future the cyst on the root of the tooth does not progress.
If the root of the tooth is to be preserved, then I advise you that its crown should be restored by the tab + crown. Naturally, this is after impeccable intra-channel preparation. As for anesthesia and your fear of pain: if they keep the tooth, they will do without anesthesia, since the “nerve” has already been removed from the tooth.If there is a need for root removal, then anesthetics of the articaine row always act flawlessly on the front group of teeth. The only thing that is a little painful is the very introduction of an anesthetic into the transitional fold (however, many experienced doctors can minimize these painful sensations).
Is it possible to die from local anesthesia after a hand test? I’m very afraid.
Hello! If we talk about modern local anesthetics (drugs of the articaine series), then there is almost no allergy to them, although sometimes there are systemic toxic reactions that cannot be prevented by any allergy tests. Thank God that at the dentist’s appointment there are many ways to prevent negative consequences even with such side effects.
Since you are asking a question about a skin test, it’s just what is done so that a person does not die of an allergy. It would be strange if a sample were prescribed in order to once again risk a person’s health. That is, you definitely will not die from a skin test. With the development of an allergy to the drug (if any), redness or slight swelling will appear on the skin, since a small dose of the drug is specially taken. However, there is no full guarantee that with a negative test for anesthetic, allergies will not develop during the administration of the drug in the form of an infiltration or conduction anesthesia during treatment or tooth extraction. It's all about the dose, the injection site, etc. A skin test is not the most perfect, there are more accurate tests. But the most important test is to take a history of allergies to certain drugs in the past. I am sure that the history of your “dental” life and general health will provide more information than tests.
Hello. Sorry, you can tell whether it is possible to remove the darkening on the tooth without drilling [link to the tooth with darkening - visible only to the doctor]. Maybe there is some kind of purge or something like that? The plot itself with darkening is smooth, not loose. Thanks in advance for your reply.
Hello! The picture is fuzzy, but it is clearly visible that the spot is black. More like carious. With this color intensity, almost always there is at least medium caries. In your case, it is located in the cervical region - a thin layer of enamel over softened tissues in this zone often does not "fly off" for a long time, determining the apparent well-being. This is due to the fact that there is no direct load on the cervical zone. This defect does not imply conservative treatment (for example, using the Icon technique), but a full-fledged tooth treatment, removal of carious tissues with subsequent filling are required.
That is, answering your question more specifically: "without drilling" will not do. Although I emphasize once again that the picture is fuzzy, and in the end, it is still up to your doctor to decide after a careful examination in the chair.
Thanks for the detailed answer. Judging by your answer, it turns out that it will be necessary to drill, because I have had this darkening for a long time (for sure, about 5 years). The doctor said that while you can observe and not drill. But I thought about modern techniques, but it turns out that the case is not mine for their application.
Hello! A month before the new year I came to a private clinic. We discovered caries on several teeth, one began to be treated. Despite being treated in a modern clinic with good anesthetics, it was painful several times. Carious tissues were removed, according to the picture they said that the nerve was very close to the healthy part of the tooth, and a temporary filling was placed. For three weeks (that’s how much it was necessary to walk with a temporary filling), the tooth did not respond to cold, nor to sweet, to anything. Removed a temporary seal, put a permanent one.Now, when I drink / eat something cold / hot, the nerve seems to “burst” a little, the pain goes away immediately, after that it does not hurt and even does not respond to this irritant for a while (usually it reacts only once I eat /I drink).
What do we have to do? Is the doctor to blame? Can waiting without treatment help? And I would also like to ask where you are, judging by your answers, you have enormous experience.
Hello, Alexander! According to your description, the doctor’s tactics as a whole are correct: first they checked, deep caries in the tooth, or already pulpitis. The fact that the tooth began to respond in spite of the positive dynamics is almost certain that this is the result of excessive grinding of enamel during correction of a seal by bite. Since the pain is irregular in nature, I am inclined to say that we are not talking about complication after treatment of deep caries. Of course, it is impossible to say 100% without verification, but I assume that nothing bad will happen next.
It would be nice to check the tooth for EDI, but few clinics have this device to determine the "health" of the pulp. Therefore, the option is to wait about 2 weeks after the treatment, but if other symptoms appear (acute pain, reaction when biting, etc.) - immediately to the doctor.
As for my work: despite the fact that I am a dental practitioner, I serve only the local attached population and do not go beyond my "province")
Good afternoon! Today I was treated with the top eight in a private clinic with an experienced doctor whom I trust. I wanted to remove it, because there was a chronic caries and it was difficult to get to it - it is from the back. But the doctor offered to treat the tooth - since it stands exactly, judging by the picture, it does not interfere with the seven and there is enough space for it.
It was difficult to treat, everyone was nervous - tooth decay was just from all sides. As a result, I found out that a nerve was immediately removed from me for one visit, but without cleaning the channels - since you simply can’t get to them. At the same time, she left some kind of “medicine” (I don’t know which one) for permanent treatment and immediately put a permanent seal.
In general, I trusted the doctor up to this point - she made me rather complex teeth, but this is the removal of a nerve without cleaning the canals and some kind of “medicine” under a permanent seal disturbs me. Should I worry?
I do not want to offend an experienced doctor, but can this be done? Perhaps you should just remove the tooth?
Hello! If "your words are written correctly", then the doctor’s tactics are incorrect. Since the channels are difficult to treat, and the cabinet is not equipped with a microscope (as an option), it was worth treating pulpitis in several visits. Partial removal of the “nerve” without the devitalizing method (pre-setting the paste that kills the “nerve”) dooms the tooth to a 100% exacerbation in the near future. The risk is very high. In addition, undeveloped canals with a partially removed "nerve" (and even with a completely removed) do not guarantee that the tooth will not become ill.
I can’t know exactly what kind of medicine the doctor put you under a permanent seal. I knew dentists who put analogs of arsenic paste already under a permanent filling, because I did not have the opportunity to treat it correctly (such a method was extremely harmful to the tooth in the future). If the doctor put something like a calcium preparation with complete removal of the “nerve” from all the channels, then the tooth can still stand with half-empty and empty channels under a sealed permanent filling, although this treatment is not promising. The resorcinol-formalin method, sometimes used by doctors for eighth teeth, is not done in 1 visit.
It is possible that a tooth should be removed or sent for treatment to a clinic where there is a microscope, but the doctor chose to block the problem - and “out of sight”.
Hello! There is a hole in the tooth, he came to dentistry, they drilled another hole in the same tooth (near the nerve), put in arsenic.They said after 2 days to come to remove arsenic, and after a week - to remove the nerve. Do these 2 procedures hurt me?
Hello! Either you are describing something wrong, or (more likely) the dentist prefers the extreme version of the routine treatment method: after extracting the arsenic paste, record separately for channel therapy. The fact is that according to the devitalization technique, after the installation of arsenic, the next visit immediately carries out endodontic treatment of the canals: it just includes the removal of the "nerve", processing and (most often) their filling. In some situations, the doctor has the right to leave an anti-inflammatory, antibacterial and (or) anesthetic in the treated canals, but I don’t understand: why remove the paste and take it separately for treatment of the canals. Perhaps not from a good life. The last question famously combines two burning topics: will it cost a lot and will the procedures be painful?
If you are treated with such methods, then I’m almost sure that it is inexpensive compared to higher-class clinics. As for pain: I can’t say anything specific, but it can be assumed. If you qualitatively killed the “nerve” with paste using this technique, and even do anesthesia at the stage of channel treatment, then it’s closer to 100%, which will not hurt or be slightly painful, but bearable. Otherwise, I can only rely on the doctor’s skills, equipment capabilities and the availability of material resources: from the level of anesthesia to the presence or absence of endodontic “lotions” (K-files, rimers, H-files, apex locator, gutta-percha, etc.).
About 3 weeks ago I did the front tooth. There was a small caries, but the doctor made a big hole, as it spread further. She said: "If she gets sick, then I’ll remove the nerve." Well, 3 weeks have passed, and only now I got sick, despite the fact that I am doing the last tooth on the right. Recently, an unfinished tooth and others on the right side began to hurt. After everything hurt, except for unfinished, and the front began to hurt. And I could not go to the doctor, since she was not there. Was the tooth sick due to those pains? Will it be necessary to remove the nerve and does it hurt?
I am now 15 years old.
Hello! In your case, the tooth may hurt due to doctor’s errors (overheating of the tooth, incorrect diagnosis, chemical burn of the pulp, etc.), or due to infection in the canals. And without additional diagnostics it is not known, one tooth is the cause of your pains, or there are several causal teeth, but the assumption is so far on the front. The search for a causative tooth is the most important stage, since without it you can hurt or do a lot of unnecessary work. I note that spontaneous pain (without irritant) of the treated tooth is a 100% indication for the removal of the “nerve”.
As for your question regarding the painfulness of the “nerve” removal procedure, pain is not excluded from a professional in the treatment of pulpitis, as a high-quality anesthesia is done. Anterior teeth in almost 100% of cases, even in medium-sized dentists, are treated without causing pain to the patient, as they are easy to anesthetize. For everything else - I can’t say so, as for some teeth the situation can be a little more complicated, and in terms of anesthesia everything is in the hands of the attending physician. In any case, you should not be afraid, and it is important to treat pulpitis as soon as possible, before he goes into periodontitis or its complications (periostitis, as an option).
Hello! Literally 3-4 days ago, the 6th upper tooth (on which the filling was placed six months ago) began to hurt very much, although at first it was not clear that it was him, because the pain was almost on the whole jaw, and I suspected that he was climbing 8- ka. But now, it seems, according to the sensations, only the 6th top hurts, and then, if you touch him, it just doesn't hurt anymore, but still I can’t eat. They said that they might remove the nerve.
Prior to that, in the same hospital, he treated caries of 5 and 6 lower teeth, had anesthesia, and as a result, I still felt not slight pain on the 6th tooth, although there was less caries than on the 5th tooth. But he suffered and healed me, it was literally this Monday, the gums still ache, and the tooth, if you suppress it, is a little felt - perhaps due to the fact that it was treated for about an hour, and even several times put anesthesia. They said that it was precisely the 6th lower one that is slightly sensitive to anesthesia and therefore it did not work much.
What needs to be done to really understand that I need to remove the nerve from the upper 6th tooth? And again, is the 6th upper tooth badly painfully treated, given that the lower 6th was not affected by anesthesia? On Monday, the doctor’s appointment has already been made. Tell me about this, what needs to be done? Plus, if you really need to remove the nerve, then do not hesitate to do this, because everything will only get worse?
Hello! I answer in order:
1. Usually acute pain, as well as a strong and long-lasting pain reaction from irritants, and all in this spirit, speaks about the appropriateness of channel treatment. It’s for a specific tooth that you definitely won’t be able to tell without a dentist - he conducts an examination and instrumental examination taking into account your, so to speak, “indications”. Often this is not enough, and a tooth snapshot and / or EDI come to the aid of a doctor, although there are not many clinics using the latter method.
2. The 6 upper tooth in comparison with the 6 lower tooth should be treated “painlessly”, but professionals do not pose the question like that - with normal hands of a doctor, all teeth are treated without pain. In the context of realities, the upper 6 tooth should be better for the average doctor if it’s not a problem at all with hands.
3. It’s definitely not worth the delay, since pulpitis smoothly passes into periodontitis and its complications (periostitis or “flux”, as it is teased by the people). Again, if you are lucky, then pulpitis can be tormented for several weeks, gradually turning into its chronic form without complications up to 6-12 months. But I do not think that it is worth hoping for such luck (I say as it is).
I am 15 years old, I’m going to be treated today. I have an open nerve, very afraid ...
Good afternoon, Svyatoslav Gennadievich. My young man has fluorosis, not in an advanced stage, but, nevertheless, there are spots. Is it treated, or will veneers only help here? And if it can be cured, then how?
Hello! The problem is not the most common, but the principle of treating spots with fluorosis most often comes down to enamel bleaching, enamel microabrasion, filling defects and making veneers. If your case is not running, it is useful to clarify about tooth whitening or enamel microabrasion.
Microabrasion removes a microscopically thin layer of enamel - in fact, this is a combination of whitening and grinding. Spot filling with light-cured composites is also an option for fluorosis for the frontal group of teeth. These are the methods that are used for mild forms of fluorosis, without the use of veneers.
Hello! Yesterday she came with acute pain, and a nerve was removed on my upper 1 on the left, before that she had been sealed 10 years ago. They took a picture both before and after. But tonight, when I click on this tooth, I feel pain. I had a bad nerve removal and need to be treated, or can the pain go away without consequences? Do I have to wait a few days before running for a consultation?
And another question: about 20 years ago, while still in school, a nerve was removed from my left 2. about 2 years ago, it darkened from the inside, and from the outside the gum turned a little blue. In a free clinic they say to me, everything is fine with him, is this really so? Why did the gum above this tooth change color?
Hello! Pain when biting a tooth is often present several days after treatment of the canals - this is the so-called post-filling reaction. Many practicing dentists consider it the norm if it lasts within 3-7 days, and when using some filling materials - up to 1-2 months. However, in this case, the pain should not be painful and should tend to decrease every day (week). Usually, the front teeth are not difficult to treat the canal, as there is one straight and wide canal in the upper central incisor.
Now about the second tooth on the left. I can only guess about the reason for the “blueing” of the gums in absentia: the formalin method or Endometasone containing formaldehyde sometimes cause such reactions. There are filling materials that cause severe darkening of the tooth and even the edges of the gums. I think that the exact answer can be given by an experienced dentist after a thorough examination of the tooth and image analysis. Including a verdict about the prospects for retreatment of this tooth.
I came to a paid dentist, said that my tooth hurt, and pointed to the bottom six. The podiatrist from the picture did not immediately see that there was a cyst on the root on this tooth, and advised me to cure the five. And she said that the pain supposedly moves from five to six. And another doctor in the same clinic two days later saw a cyst on the six. Removed the bottom 6 with a cyst. At that time, the five were already beginning to heal. Now I'm flying the bottom 5. They put anesthesia for two days to remove the nerve - nothing helps, anesthesia does not work, the tooth hurts terribly. Arsenic was put at night, released home for a day. A day later she came - arsenic did not work, they again set anesthesia. In general, nothing helped.
It so happened that the nerve was pulled out to me at the very moment when the tooth was removed - 15 minutes after the extraction. And even under that anesthetic it hurt me. Then they let go home for a couple of days with an open tooth completely. A couple of days later she came, they cleaned the channels again and sealed me. The pain while cleaning the canal was terrible at one point, somewhere in the middle of the canal. And at the top of the canal it was no longer painful. And the pain that appeared during the cleaning, and remained. Now my tooth hurts every day, a week has passed. After 6 pm and at night the pain increases. I saw the picture myself - there is one channel, and the picture is sealed normally. The doctor also says that everything is fine. In general, I do not know what to do, the week has passed, and the tooth hurts. There is a temporary seal.
Another therapist in the same clinic suggested that there is a nerve process that can be seen in a 3D image and put me a resodent. The next day, the pain also continued, came back to the clinic, already there was a change of the third therapist. The third therapist examined the hole, examined the closer teeth and in the picture I saw caries already in the fourth and third tooth - a hidden caries that is not visible with the eye, it is inside under the crown of the tooth. And after that he made the assumption that my five was sealed normally, but it’s good, the nerve appendix is not left there, and the fourth tooth next to it may hurt and supposedly give to the five. But I specifically have 5 tooth pains - according to my sensation, during the day it aches, itches from the inside, bursts with it, I just want to rip off a temporary seal, pick everything in this one channel. In addition to all this, the gum inflamed: under the remote 6th, and under the 5th and comes to the 4th. By evening, the pain intensifies, and when I go outside, with every step in my fifth tooth I feel as if it were pulling, and he shoots.
I have been drinking it for 2 weeks. I don’t even know what to do. In the fifth tooth, the canal was filled on 02.21.17. Today is 02/28/17. Tomorrow I need to go to this clinic again for an examination. There was such a situation that three doctors are in the same clinic, and they have different opinions. And my teeth are alone. What could it be? What to do? ((
I want to note that before this 5 tooth was touched, he was NOT sick, and only 6 with a cyst were sick.
Hello! Thank you for describing in such detail. You are actually right: there is a suspicion that there are more pain in the hole, and the fifth tooth could have nothing to do with it. That is, alveolitis could begin, and post-filling pain in the treated fifth tooth also intensified the symptoms. This strange, so to speak, “tandem” to some extent could confuse doctors. I do not do this in my practice, since this exacerbates the treatment, or rather, leads to deterioration more often. Not only is removal a trauma, but also after canal treatment, many dentists get the same trauma, but only periodontal damage, against the background of a number of shortcomings.
If you send a snapshot of the tooth after the canal treatment, then I could analyze the quality of the treatment. In the meantime, I’ll just say in absentia that it’s worth taking care of the hole, alleviating this symptomatology, and then checking the fact of a good treatment of the fifth tooth canal. If you continue to look for non-existent problems by other dentists, this is fraught with multiple useless dental treatment and, God forbid, their removal, which with some dexterity is practiced by dentists who "chop off the shoulder." So start with the hole, make sure the quality of the fifth treatment, and then look at the situation.
Hello, Svyatoslav Gennadievich! I really need to evaluate the result of canal treatment and further prognosis. The bottom six, periodontitis. The treatment process: metapex for a week, filling with the method of vertical condensation, another week later a permanent filling. In the picture I see the filling material and the gutta behind the apexes. Are there any other errors besides this? The doctor said that he deduced specifically "for the purpose of treating inflammation", so she did not begin to ask him other questions. How tightly sealed are the channels? Confuses the uneven color of the filling near the top of one of the roots. And in general, how do you rate this result?
At the moment (2 weeks after setting a permanent filling), sudden aching pain (1 time in 2 days), independent of load, irritants and time of day. Sensitivity decreases, chew soft foods calmly.
I apologize for the many questions, but I, as the owner of already three “dead” sixes, really want to understand the mysteries of endodontics. Thank you in advance for your answers! Snapshot: [link visible only to the doctor]
Hello! You say everything correctly: there is a conclusion of the material, a slight inhomogeneity (unevenness of the material, but not much). However, such a filling is not bad in medical circles, and its consequences will most likely not be negative. It's just that with periodontitis it is important that the obstruction of the canals is tight, so that the apical openings are blocked. The biggest “sin” for a doctor would be if the apical delta were left without material. Then colleagues would have lifted him to the pitchfork, and much more would have been done. And so, from the point of view of the medical community - a very decent filling. Another issue that is not always comfortable for the patient: often you have to wait long enough for all the symptoms to go away (post-filling pains can last up to 2-3 months in such cases). It bothers me that you have a sudden aching pain with a certain frequency. Although, perhaps, this is such an individual reaction (you can still evaluate the adjacent tooth for caries, as an option). But the picture can only sympathize with you, and in a sense praise the doctor that everything has been done as close as possible to the ideal for periodontitis.
Thank you so much for the quick reply! You all "sorted it out" and returned my trust in my doctor, and I was thinking of changing the specialist, since the retreatment of the canals of two more problematic sixes is coming up. Before your answer, having seen enough pictures of beautiful and graceful endos on the Internet, my tooth seemed barbarously crafted to me)
Regarding pain: on the next seven, a deep filling was replaced, and this tooth is under suspicion as a cause of pain, although subjectively it is absolutely calm. While watching. Thanks again and success! Sincerely.
Svyatoslav Gennadievich, I’m 17 years old, I have this problem: they filled me up on my nerve. And now I touch only to the tooth - it starts to hurt. And in general, without touching it hurts like that, and even reacts strongly to cold and hot. And it’s hard to sleep. Give some advice, please!
Hello! I believe that the channels, judging by the symptoms, were not treated, that is, the "nerve" was not removed. You describe the symptoms of pulpitis that appeared after installing the seal, that is, in this case, full-fledged endodontic care is required. I recommend contacting the same or a different dentist-therapist for the treatment of canals. The search for a causative tooth is mandatory: the adjacent tooth sometimes starts to hurt, but it is felt that the treated one hurts. So urgently to the doctor, so as not to wait for complications.
Svyatoslav Gennadievich, I contacted you recently and I want to ask one more question. For a week the tooth hurt and stopped hurting, what should I do? I think the nerve is dead - could it be by itself if there was an inflamed nerve? And is it dangerous if the nerve is dead, do you need to go to the dentist as quickly as possible? And I wanted to ask: if I go to his appointment, what can I say because he will ask what is the problem?
Hello! Given that you had spontaneous pains that persisted for a long time and did not allow you to sleep normally, it was highly likely that there was a complication that occurred after the treatment of caries. That is, it was an acute stage of pulpitis. Currently, it is a chronic form, so the tooth has stopped responding. If the "nerve" quickly dies, then a purulent form of periodontitis may begin in the near future. In the case when the compensation prevails, the “nerve” inside the channels may be in a stage of inflammation for a long time, but its death does not occur, therefore, there may be an aggravation of pulpitis in the future, or the same scenario will happen as I described earlier: the “nerve” will die and the tooth goes into the periodontitis phase. Be that as it may, it makes no sense to wait until the tooth aches again.
If you come to the dentist’s appointment, you need to say exactly what you described above. This is enough to have a reason to depulpate the tooth and prevent the negative consequences of an infectious origin.
My question is: often after a visit to the dental office herpes appears on the lips. A week ago, the nerve was removed, the canal was filled, a temporary seal was placed. Tomorrow go to the doctor, put a permanent seal, and I have herpes. What to do?
Hello! Labial herpes is one of the most common diseases, the trigger of which is a decrease in immunity (including due to stress, in this case in the context of a visit to the dentist). Most often, this disease is not an obstacle to dental treatment. An ideal option is the use of drugs for the rapid relief of herpes symptoms - antiviral therapy with acyclovir-containing drugs. With the frequent occurrence of herpes, patients often themselves know what is ideal for them, since they have “eaten the dog” in this matter over their lives. So be sure to go to the doctor, and the dentist himself will find a way out.
Hello, my name is Yana. I am 12 years old. On March 28, they put arsenic on me, as it was very painful. Today came, but again it hurt me and again arsenic. Will it hurt to remove the nerve?
They will do everything for me without pain medication. Lower tooth, molar. Very scary.
Hello! You yourself have refused painkillers or are you just panicky afraid of anesthesia injections? If this is not the case, then ask your doctor for a good anesthesia to make the treatment painless. However, lower molars are sometimes difficult to treat for a number of reasons, and anesthesia at your age does not always work adequately. Be that as it may, be patient and ask your doctor to work with anesthesia.
Do not be afraid. Keep in mind that canal treatment is a very crucial moment: if you do not carry it out qualitatively, then the tooth can be lost in the next 1-5 years. But he is already permanent, so there is something to fight for. Good luck with this event!
A week tooth ached! Then he passed. Then I went to the dentist, told him that the tooth hurt for a week. He knocked and said that if he was ill, come. And he said: maybe it slipped through ?! Describe my problem, please.
Hello! Apparently, the dentist for some reason can not or does not want to conduct timely diagnosis of a problem tooth and suggests waiting for the weather near the sea - when the tooth is sore, the gum swells, etc., that is, when, it is possible, to save the tooth it will be difficult or even impossible.
If the doctor does not have the necessary diagnostic devices, tools, experience, desire or time, then they often say: "Come back later." From the description of the symptoms alone, it’s hard to guess what’s happening with your tooth: pulpitis, periodontitis, exacerbation of periodontitis in a tooth already treated in the canals (channel) or something else. An X-ray (or on a visiograph) of the suspicious teeth might clarify something.
Look for a causative tooth at a normal dentist and treat it soon. It seems that you know the approximate localization of a diseased tooth - you need to take pictures of this area and see what is wrong there.
Hello, a week ago, a nerve was removed from the front tooth. She was treated in a private clinic. The check indicated that they made filling of 1 channel with lateral condensation and put a light seal. I would like to know if the tooth will collapse quickly and is it possible to somehow delay it?
Hello! If the doctor has done everything as expected, and the tooth has sufficiently strong supporting walls, then without a tab (crown), based on only therapeutic treatment, it can stand for more than 10-15 years. Every 1-2 years the seal should be inspected, make corrections, check the state of the root in the picture. Each doctor has his own point of view on control examinations. Someone believes that they are not needed at all. Personally, I am of the opinion that it is better to do the first inspection of the seal in six months, the second in 2 years, and the third in 4-5 years. Although, I repeat, each doctor has his own opinion on how carefully and often you need to monitor the treatment.
Hello! The last molar (7) broke off very strongly after a filling had fallen out of it. The doctor said that in the end it is necessary to remove the nerve, clean the canals and put a permanent seal. At the moment, he laid down the medicine for 10 days and put a temporary seal. The tooth did not hurt (and when it broke away, both before and after - only a little ached on the first day, but not at all critical). On the second day, a slight irritation appeared on the gum, because the filling touches it (the tooth broke off under the gum itself), and the tongue. It does not hurt, but it nibbles noticeably. The irritation does not get stronger, but the question is whether this is normal?
Hello! Not quite normal. It is best to adjust the temporary dressing lying on the gum, or to immediately treat the canals if it is impossible to carry out the correction. This is due to the fact that non-arsenic paste irritates the mucous membrane and can even create a burn. And 10 days is not a fundamental need. This paste, according to the instructions, is put from three or more days. That is, it is not necessary to boil a tooth in its own juice.
Hello, I’m 13 years old, why did they put arsenic on me, but the nerve didn’t die? In the clinic, they removed the old arsenic, looked, but my nerve did not die. They said that again arsenic is needed. Imposed a new arsenic. But he hurts me, but bearable. If the nerve does not die, what will dentists do to me? Tell me please.
Hello! The fact is that at a certain age of the patient (up to about 18 years old) anesthesia is difficult for some doctors, but this is only due to a lack of professionalism and working conditions, especially in polyclinics, where many people need to be served in a short time (almost not three in one hour). That is, in terms of anesthesia and such a routine method of maintaining a pulpitis tooth, the clinic often does not provide a high-quality service.
Often in clinics, the following classical pattern is observed: arsenic, still arsenic, painful canal treatment, medicine (antiseptic), another medicine, canal filling, then filling, again the return of pain, retreatment with medication, and often tooth extraction if the above procedures are ineffective. Of course, there are many doctors in hospitals and polyclinics who give quality despite the severity of work in this system, but, in my opinion, your case does not fall into this category.
That is why I can say that if "the nerve does not die," the doctor will do the job as high quality as you give him. If it hurts too much and you interfere with the doctor, then he will do as it turns out, and then - see the above scheme.
Therefore, I recommend changing the doctor to increase the level of treatment. I think that the doctor who repeatedly puts this “arsenic” to you will still be grateful to you, since he obviously can’t cope with the requirements of modern treatment techniques in dentistry.
Hello. And here I have such a problem. The lower chewing tooth on the right (the second from the end) fell ill. It had a seal. Replaced. Still sick. She came again, they removed 3 nerves, something was covered up and told to be like for several days.
Today, something was picked and sealed. But now, by the evening, he became quite ill. This is normal? After all, there are no nerves anymore ... Why can he get sick? And if this is the norm, then after what period should it cease to hurt? I'm afraid that something could have done wrong. When and in which case to sound the alarm?
Hello! In the first days after channel treatment, there may be so-called post-filling pain. This is also considered a symptom of a complication, but its severity is determined by analyzing the image, at least. Often, it is not necessary to re-treat the tooth, as the doctor’s small errors stop over time, and the symptoms disappear on average in 7-12 days.
However, sometimes the doctor makes significant mistakes during treatment:
1. Too much aggressive material leads to the apex of the root or roots of the tooth;
2. Leaves a tool fragment in the channel;
3. Performs perforation of the tooth wall;
4. Does not go to the end of the channel or channels, etc.
All this can be seen in the picture. In such cases, the doctor must redo his work. Otherwise, the prospect of waiting for trouble from new exacerbations in the form of pain, swelling, temperature (with the risk of tooth extraction in the near future).So if the pain will increase or will not pass for a long time, then it’s worth the alarm, since we don’t know how well the work in the channels was done.
Hello, today I went to the dentist to treat a “chewing” tooth - he pulled out the remnants of food from there and put a temporary filling. He did not say anything to me, except that to come in a week and that’s all! Will I have a nerve removed from my tooth? Please tell me! Very scary (
Hello! Judging by your description, we are probably talking about a two-stage diagnosis of deep caries. When the doctor doubts whether the patient has caries or pulpitis, he can put a temporary filling and wait for a while. If you come according to plan or earlier and say that a tooth closed with a temporary filling is very painful, then this is pulpitis - the canals are treated according to this protocol. If there are no symptoms, the doctor will routinely treat deep caries.
You are afraid to remove the “nerve” from the tooth, and I would be afraid of incorrect diagnosis, since such a check is not without errors. Much more promising, faster and more accurate - this is EDI (electroodontodiagnosis) using the device.
All, of course, is good with painkillers, but what if they are allergic (tested for 12 main ones)? And even a single analysis showed that “everything is fine” - they injected, and pumped out for 4 hours. There was no question of treatment. The doctor put "arsenic", without a guarantee that it would not hurt. I have a low sensitivity threshold. Tomorrow to the dentist, in the hospital there are no modern drugs, and what to do? How old-fashioned - 100 grams and a hammer ?!
Hello! If we are really talking about allergies and you are intolerant of Lidocaine and articaine drugs, then the situation is difficult. However, questions remain: what anesthetics have not yet been tested? Why do you say that you tested on 12 essential ones, and then you talk about modern anesthetics in the hospital, having hope for their use?
About the fact that you need to go to the dentist under the "chauffeur" - definitely do not need to do this.
Back in Soviet times, there were protocols for the management of pulpitis without anesthesia, moreover, it was quite reasonable and often with minimal pain. This was done as follows. Almost always with pulpitis, we have a tooth decayed by caries, there is a carious cavity with softened dentin. Accordingly, millimeters or even fractions of a millimeter remain before the pulp. The doctor’s work is carried out with air-water cooling. That is, a lot of water is exposed, which allows using a brand new boron to accurately make access to the pulp, where the paste based on paraformaldehyde (non-arsenic) is placed for 3-5 days. On the second visit, the canals are usually already treated painlessly.
In the presence of pain, modern approaches to the treatment of pulpitis suggest that anesthesia is done intracanally (intrapuloparially), but carefully so as to exclude an extra "spill" of anesthesia. With due dexterity of the doctor, there is a feeling of fullness in each channel for 1-2 seconds, after which it is possible to carry out mechanical and drug treatment of the channels for a set hour or more, taper them and fill them - no sensations will appear. The meaning of intra-pulp anesthesia in your case is that the dose of anesthetic is minimal (negligible) and practically does not go beyond the canal, which means that the risk of allergies is reduced to almost zero. This makes it possible using this method to do the job efficiently and with minimal pain.
Hello, yesterday I was treated with a tooth, seven at the top. They removed the nerves, sealed the canals and put a temporary seal. They said to come on Monday, they will do permanent.But the fact is that the tooth itself does not hurt, but it is very painful when bitten, when I eat and when it comes into contact with the lower tooth (when I ate, I cried out in pain). What could it be?
Hello! Apparently, in your case we are talking about post-filling pains, which are sometimes observed after treatment of tooth canals. The causes can be various errors and inaccuracies during the treatment of channels: from gross to insignificant. For example, perforation of the root or bottom of the tooth crown, removal of the filling material beyond the apex, leaving the instrument in the canal without proper correction of the situation, the passage of the canal or part of it (or, in general, one canal was not found), periodontal burn during rough drug treatment of canals under significant pressure, etc.
In some cases, the causes of pain when biting on a tooth are several at once, but in order to understand the severity of the situation, it is important to analyze the image of the tooth before, during and after filling. The last version of the tooth images with already sealed canals should be made in different projections (this is desirable). That is, pictures (for example, on a visiograph) are taken from different angles so as not to miss the doctor’s mistakes, which will indicate the cause of the pain.
If it turns out that all the channels were found and sealed perfectly, there are no debris, perforations and other serious problems in them, then we can safely expect that within 4-7 days the pain will disappear with the prospect of preserving the tooth for many years. In the case when the material is removed at the apex of the root, the pain often persists for up to 2-3 weeks and even several months. Sometimes the discomfort lasts for years, and some patients cannot stand it and require a tooth with a large “conglomerate” to be removed behind the apex (in the most difficult clinical cases).
When there is not much material outside the root, then most often the pain disappears within 1-2 weeks, and the tooth no longer makes itself felt, although this situation is also considered by some experts as a complication after treatment.
Perforation of the tooth wall, fracture of the instrument, removal of filling material into the maxillary sinus, mandibular canal, in large quantities per apex, canal or canals not passed, etc. - all this will require retreatment, and in severe cases, tooth extraction or other surgical intervention. So to understand what kind of problem you have, snapshots are required.
The first time was at the dentist. Turned to a paid private clinic. After the injection, the nerve was removed, it was very painful. Then they put a temporary seal. On the second visit, they also cleaned the canals after the injection, it was painful again, but the most painful thing was when the seal was squeezed out into the canals, hellish pain! And then for some reason they put a temporary seal on top, and before that they watered with some kind of medicine. Now, it seems, it does not hurt, but the third time I’m very afraid to go.
Maybe it makes sense in another clinic to take a picture and consult?
Hello! If there was pulpitis and it is really about removing the “nerve”, then I don’t understand why you are not affected by anesthesia and why the tooth is treated in such a large number of visits. I’m almost sure from these two signs (I repeat, if the diagnosis is pulpitis) that the doctor cannot cope with some difficult situation and tries to stop it, as far as possible, in order to save the tooth.
Just in this vein, it makes sense to get a consultation in another clinic.
Hello. I came to the dentist in the state polyclinic because two small holes appeared on the filling of the lower penultimate tooth on the right, and the filling itself began to collapse (because it’s old). The tooth didn’t really bother, it just ached sometimes. The dentist opened the seal without any x-rays, and began to pick it there.It became very painful, and he did anesthesia. After that, he picked something else and put, as he said, arsenic. I appointed the next appointment in five days to remove it.
Throughout all five days, the tooth ached and hurt, the pain intensified every day, and at night it was simply unbearable. In a calm state, he ached and jerked, and when biting, sharp pain appeared. Today, arsenic was removed, although the dentist simply opened the canals, in other places this white nonsense remained. To my proposal to take an X-ray, he refused, saying that it was not necessary. He told me to come in a week later for filling, and to close the hole with cotton wool during meals. Rinse your mouth five to six times daily with a solution of soda, salt and iodine. Is it possible to walk with so many open nerves for so long? Isn’t it dangerous to give a doctor blind work like this? Tooth, by the way, did not become easier. It hurts, even to tears. I just can’t stand the week. I think already to go to another specialist.
Hello! You think in the right direction: the doctor practices a routine method of treatment for obvious reasons (the state polyclinic nevertheless). Walking with open canals in the tooth is not recommended. The fact that the treatment is currently ineffective is quite natural: the tactics of working with pulpitis are incorrect, arsenic paste is not put at all today because of its harmful effect on periodontium, and you can’t go with it for 5 days in principle. Appointed rinses are symptomatic therapy. It is carried out sometimes when the doctor has carried out adequate treatment in the canals, but now this is not visible.
I recommend changing your doctor (and it is quite possible that this will be a great relief for your current doctor).
He was at the dentist’s, he treated the top six. They started to clean the caries itself, then put the arsenic, released it for 4 days. Then he came, again they began to drill - apparently, on the first visit, caries was not completely removed. So - they started to remove the nerve, without an injection, the attempts to hook the nerve themselves were tolerant, but when the nerve was hooked, it became sooo painful, darkened in the eyes, thrown into the heat, the pressure decreased. They did not begin to fill, citing the smell of pus, they said rinse with soda, drink antibacterial pills and come on Tuesday to put the medicine directly from the pus itself (like that). Will they put the medicine painlessly? Or will there again be wild pains when trying to stupidly clean or check for pus with a needle at the base of the tooth? Was the nerve that was removed the only one? Since now the tooth does not respond to cold and hot food, to absorption. And what is supposed to happen after setting the medicine?
I am 16 years old, I am treating my teeth directly at the municipal hospital. As for anesthesia - he took ultracaine on the first visit, the dentist gave an injection on one side of the tooth, that is, from the side of the cheek. I heard that it’s better to chop off the tooth on both sides, for more action.
It is also necessary to remove the tooth, the upper six, on the other hand, but there the doctor himself sells anesthetics. Friends said that the tooth was completely numb, and there was no pain or discomfort when the tooth was removed, only a slight crunch. I hope that it will be the same in my case.
Also wanted to know in which cases the nerve removal itself is prescribed? Only with pulpitis, as I understood, based on reviews. How to independently determine pulpitis by external factors? Thanks.
Hello! There are many questions, I will begin in order. Firstly, you strangely mixed in a bunch the nuances of treating pulpitis and periodontitis. With pulpitis, there can be no pus in the canals (except for pediatric dentistry in rare cases), and with periodontitis they do not put “arsenic” and similar pastes in order to kill the “nerve”, since it has already died in all channels (in the sixth upper teeth often have 4 channels, a little less often - three).
As for the diagnosis in your description, I can’t give a definite answer: you describe the pain during removal of the “nerve” from the canal, and then talk about the “smell of pus”. This is strange. I do not exclude that you had gangrenous pulpitis, where the pulp decomposed only in the coronal part, and remained alive in the canals.
The fact that the paste for devitalization did not work adequately does not mitigate the guilt of a doctor who cannot conduct normal anesthesia. It is most often done for the upper sixth teeth not only from the buccal (infiltration), but also from the palatine side (palatal conductor). Thus, with the help of the articaine preparation, complete anesthesia is achieved.
From your description, I don’t understand what the difference is between when the doctor performs anesthesia with Ultracain and the option to remove the tooth with the anesthetic, which the doctor sells.
Removal of the “nerve” is one of the stages of the treatment of pulpitis, and with periodontitis, as I have already noted, the “nerve”, as such, almost always does not exist. In extreme cases, it is a necrotic piece of flesh that has already begun to decompose.
Judging by your description, I would strongly recommend changing the doctor.
Good afternoon. Recently, they put a medicine on my 6th tooth from the bottom (to kill a nerve) and next Sunday they have to remove the “nerve”. But the fact is that anesthesia practically does not affect me: they tried a conductor, which, as the doctor said, should completely deprive sensitivity. As a result, there was only a very slight numbness. After that, several more injections were made, and one of them was even painful after the previous anesthesia and was made, as it were, inside the tooth. Only after the third such injection did it not hurt exactly to the extent that I did not jump out of the chair (I have a very low pain threshold). Tell me, how painful it will be to remove the nerve and is there a way to completely anesthetize the tooth? Because the last time they did not achieve complete pain relief, and the upcoming procedure, as I understand it, is even more painful.
Hello! I think that the dentist has a discord for the dentist: it is possible to achieve persistent anesthesia of any tooth by numerous methods, ranging from infiltration and conduction anesthesia to intraligamentary and intra-pulp (at the second stage of treatment, as an option). If the doctor can’t anesthetize, this more often indicates the incompetence of the doctor, much less often - the impossibility of pain relief specifically for this patient. Moreover, each dentist has his own baggage of knowledge in the field of anesthesia, and often it is not enough for people with a “low pain defect”. However, I know many cases when intraligamental anesthesia helped out in the most seemingly hopeless attempts to anesthetize a tooth well.
It’s strange that you were given anesthesia inside the tooth and at the same time they put a paste to devitalize the “nerve”. According to your description, there are doubts about the competence of the dentist. I recommend not to torment yourself or the doctor, but try to contact another specialist. As a rule, a good doctor is best suited (you need to ask friends), working in a private structure for more than 10 years, but less than 30 years. It is useful to keep in mind that the “old guard” of dentists once practiced live treatment, and there is a danger that skills in working with anesthetics have not been improved.
Hello, I always had a problem with my teeth. And now, going to the dentist threatens to occupy the office of this month for two. The fact is that I am very worried about the incomprehensible process, which I touch with my tongue. The upper tooth (probably the seventh) is half destroyed (and inside), only a piece of the crown in front has remained, but quite large, I can’t see what kind of strange process is there.If you try to crush or move it, then the growing pain, very strong, immediately begins to spread, it immediately gives off both the lower teeth and the upper (on the right side). It can not be a nerve? He is inside the tooth. But what I can’t imagine.
Hello! Judging by the description, you have only one root (roots) of the upper chewing tooth left. The described "process" can be:
1. The gum, which draws in an empty space, covering the root;
2. Granulations that sprouted through the tooth decay destroyed by caries. Granulation is a consequence of inflammation in the root (s);
3. Pulp hypertrophy (extremely rare). More common in childhood, when the tissue of the “nerve” sprouts from the crown of the destroyed tooth and occupies free space.
I advise you to urgently consult a dentist: most likely, you will have to remove the roots of the tooth, but you never know what - suddenly there is still a chance to save the tooth (carry out treatment in the canals and restore its crown to restore the tooth lost function).
Hello. Today they removed a nerve in my lower tooth (right side, penultimate tooth). Anesthesia did not work. But the worst thing is that I’ll still go. The doctor said that you need to put the crown, as the tooth is damaged by more than 60%. First you need to measure the size, then it will be set. Please tell me, will it not hurt to put this crown?
Hello! The fact that anesthesia did not work is closer to the dentist’s 100% fault. As for fitting and fixing crowns - most often this procedure does not require anesthesia, in rare cases, application anesthesia is enough to get anesthesia of the regional gums for a short time. So your worries about crowns prosthetics are in vain, but I advise for the future for channel therapy (especially the lower molars) to find an experienced dentist from the point of view of working with anesthetics.
Hello! I am 17 years old. She underwent a medical examination for admission to a medical university in a district clinic. They said that on 47 tooth there is superficial caries that needs to be treated. We checked all other fillings that were placed in the same clinic for 2-4 years - everything is normal.
On the 25th, a tooth fell in the lower right. I admit, I sinned at 47, but I understood intellectually that from light caries I can’t be so sick. The pain, by the way, was not very acute. Rather, it was pulling and aching, but after some time it passed and then again the tooth began to ache. The next day I went to the clinic to the doctor. 47 teeth were immediately excluded, but 46 interested the doctors. Since 2014, there has been a seal on it (depth 1-1.5 mm). They made an x-ray - in principle, everything is in order, but some place was of interest to the doctors, so they decided to remove the seal. They took off, looked - everything is fine, the bottom is clean. They set a temporary one and told me to come on the 31st to see what and how (it didn’t work out before - left before Sunday). The doctor said that he suspects pulpitis, but so far will not do anything.
Today I went to the reception. These days, the tooth was still a little crawling, pulling, but there was no direct pain that even climb on the wall. She even managed without pain medication. The doctor confirmed the diagnosis and said that he would remove the nerve. Today he drilled, laid arsenic and said to come to him in a week to remove and install a temporary seal.
Could you answer how serious this procedure is? I understand that pulpitis is a dangerous disease, but it is the consequences that interest me. Just the next day we’re going to relax at sea and I wonder if I can swim right away, or will I have to wait so as not to cause inflammation? If it’s important, I can tolerate anesthesia well, I don’t feel pain, although I am treating my teeth in regional dentistry.I also trust doctors - in the spring they simply saved me from pericoronitis, and before that they treated me for deep caries and even preserved my nerve.
Thank you very much in advance )
Hello! It’s great that you have a positive attitude towards treatment. Pulpitis is not directly a dangerous disease, but if it is ignored, it goes into diseases that are associated with purulent processes in the bone tissue, which really poses a threat to health and even life. I think that it is advisable to treat the canals and fill the tooth before your vacation at sea. It is undesirable to go with the paste installed for devitalization, since the “nerve” under this paste can begin to decompose (especially if the rest is delayed for reasons beyond your control), which, in turn, can lead to undesirable consequences.
Hello! The question is this. There is caries on the central incisor of the upper jaw, a small piece of enamel has broken off from behind, there is no pain, the tooth didn’t bother earlier either. The doctor said that due to extensive caries during the cleaning process, the pulp chamber will open and you will have to remove the nerve. You can remove the nerve in one go (because there is only one canal in this tooth), i.e. remove caries, remove the nerve, clean the canal, expand, seal the canal with gutta-percha pins and the tooth itself is already a permanent filling. What confuses me is that the seal is planned to be installed immediately constant, immediately after filling the canal, while at the same time there is no x-ray diagnostics. Those. before all the manipulations + for checking the length of the channel (using K-files, but I also don’t know if the doctor has an apex locator) + after filling the channels with gutta-percha, an x-ray is not done. But the seal is already immediately fixed. I heard that mistakes during canal treatment are very common - overfilling, underfilling, which leads to serious complications. And then immediately permanent, and indeed, removal of the nerve, treatment of the channels without any x-ray control.
Is it worth it to do all this without x-ray control, or is it worth looking for a clinic where they do this control? Is it mandatory in the treatment of a single-channel tooth?
Hello! You are right: according to the protocol of endodontic treatment of a tooth, an x-ray is performed both at the stage of diagnosis and after filling. These requirements, in fact, are mandatory, but modern realities are such that in a number of clinics (often budget) it is not possible to conduct this type of diagnosis. In addition, in many respects, the treatment of one channel of the upper central incisors usually does not cause difficulties, and in almost 95% of cases everything is successful, therefore the fact of monitoring in such cases is something like a formality, a protocol requirement. This is from the point of view of the classical treatment option, when the doctor, having extensive experience and a good level of knowledge, does not encounter force majeure situations in endodontics. Otherwise, an x-ray is required even at an intermediate stage (with tools introduced into the channel to determine the channel curvature, passage depth, the presence of a “false” direction, etc.).
Bottom line: although errors in the treatment of central upper incisors are rare, if you have any doubts about the doctor’s competence, I recommend that you still make a control shot.
I have pulpitis on my 26 tooth, the doctor is already changing the 3rd temporary filling. Today she pulled out a nerve without anesthesia, it was painful, she said that it was a narrow channel and it was necessary to expand it for a long time. She wrote me down the next day. I asked, maybe it’s better with an injection, since it hurts, to which she replied that the pain will pass as soon as the nerve is pulled out, and there is no need for this. Maybe better with anesthesia? Tell me ...
Hello! Your doctor practices dubious methods of treatment - it is more advisable to carry out treatment with high-quality anesthesia in one visit.That is, the removal of the "nerve" in the first visit is carried out without laying any preparations in the tooth. The fact that the doctor does not use anesthesia even if you have a desire for it is, in general, strange - it is, at least, inhumane in relation to the patient.
I advise you to find another dentist.
After arsenic, the tooth inflamed, what should I do?
Hello! If it was really about the use of arsenic paste, then you may need to carry out anti-inflammatory treatment, as there is a risk of developing arsenic periodontitis in the future, which is fraught with complications - up to the loss of a tooth even with seemingly high-quality processing of the canals.
For the future, I advise you not to go to dentists who practice using the arsenic layer to devitalize the tooth “nerve” (numerous studies have shown the harm from the use of such pastes, and today they use alternative devitalizing preparations that do not contain arsenic).
Hello, Svyatoslav Gennadievich. Tooth, top 6. I started to get sick, I went to the doctor, she looked, took X-ray pictures, and eventually put some kind of medicine. Which one, she did not say, and somehow I was not interested. I did not drill anything. She said that there’s a hole already. Further, I recorded a day later to come.
What will they do to me? Will nerves be removed? Will it hurt me? I’ve been doing the bottom six for a long time ... I removed my nerves, cleaned the channels, the pain was terrible. I'm afraid now. Answer please. Tomorrow at the reception at one in the afternoon.
Hello! I think that they put a paste for devitalization in order to delay the treatment of the canals of the upper sixth tooth. With a high degree of probability, the "nerve" was already opened. Due to lack of time or for other reasons, the doctor put a paste to treat for the next visit.
As for the pain when removing the "nerve": when compared with the lower tooth, the upper teeth are anesthetized many times better, even with an average level of skills at the dentist. But under certain conditions, you can not “freeze” the top six to a sufficient degree. I hope that your dentist will cope with this task and not make you suffer. Good luck
I had a perfectly healthy tooth, without caries, but the doctor decided to depulpate it in order to put a crown. The crown has not yet been placed, it should go in two days, but the tooth began to hurt when tapped. I don’t know what to do ... The doctor took the money, he said he would do it cheaper. Where and to whom to contact, I do not understand. I hurried with the doctor.
Hello! I think that the doctor did not inform you about possible post-filling pains (they are observed very often). Technical errors made during endodontic tooth treatment are not excluded. In any case, while you should not blame the doctor, you need to take a picture and get advice in another clinic. It is possible that in fact everything is in order, and you just need to wait a short time - most often the pain disappears 4-7 days after the treatment of the canals.
Toothpulpation for certain types of crowns (for example, for cermets) is most often advisable due to the large processing of the tooth under the crown. So do not rush to conclusions and once again carry out a tooth diagnosis for possible medical errors, and from this point of view it will already be possible to talk about future plans for the tooth.
Svyatoslav Gennadevich, read all your answers to the comments. Thank you so much human for the work done and the time spent! Thank you for not leaving us unattended! I bow to you.
I support! )))
Good morning, Svyatoslav Gennadievich. Tell me, I read everywhere about such symptoms of pulpitis as spontaneous bouts of pain (usually they write about long bouts, 5-10 minutes or more), or about aching pain (constant or periodic, including throbbing pain), an increased reaction to temperature (if the nerve is still started to become inflamed). And what can mean short-term shots in the tooth (they are very short, literally fractions of a second). Arise spontaneously. Sometimes rare: 2-3 times a day (although stronger), and sometimes more often, for example every 15-20 minutes, but already weaker (sometimes almost invisible if the day). At night, it does not bother much, rather in the evening. There is caries on the tooth, but it is definitely not deep (in the picture, too, no hidden cavities are visible). Such shootings have been going on for a month. Shoots periodically in other teeth (including depulped). A tooth does not respond to temperature (more precisely, it reacts like a normal healthy tooth). When eating food, too, no pain. All shootings / tingling are exceptionally short and spontaneous.
Thanks!
Hello! Even taking into account the nuances you described, the symptoms are more like a complication of caries (pulpitis rather than periodontitis). If the pain occurs without irritants and, moreover, has a certain regularity, especially taking into account the evening time, then this is closer to 100% pulpitis. Sometimes the ripple also occurs with periodontitis. When eating food amid complications of caries, sometimes there is no pain reaction. If in doubt, you can check the tooth on the EDI device to find out if the pulp is healthy, inflamed and has begun to die or has already died. Although this device is not available in all dentists.
Still, I recommend contacting a dentist (possibly even several specialists) to clarify the situation, determine the problem tooth and plan treatment.
Hello! When treating pulpitis, one of the canals was not completely cleared (a little more was left on the tip), but the nerve itself, as I understood, was dead. The doctor tried again the next day to clear my canal, but the picture showed the same thing. The doctor said that it is pointless to do something, and the tool simply can not get in there. Can you continue to live with such a tooth, or should you contact another specialist? The tooth itself does not hurt. Thank you
Hello, Catherine. If you do not clean and seal the canal to the end, then in fact the void remains in the place where the pulp was, and microorganisms can begin to develop there, which subsequently very often leads to inflammation of the tissues near the root of the tooth. The tooth canal should be cleaned and sealed to the apex - this is a necessary criterion for quality treatment. An incomplete canal is a source of infection, and the risk of inflammation in this case is very high.
With complex canals, endodontic treatment is best done under a microscope; in the absence of such equipment, the doctor may not be able to cope with the treatment. I strongly recommend that you contact another specialist for canal treatment, having previously specified whether the clinic has the opportunity to carry out treatment using a microscope.
My tooth ached for a very long time after removing the nerve. It was either closed with a temporary seal or opened because it was starting to hurt. And they took a picture, and they said that everything was fine. Today I went to them again - they took a picture, cleaned the channels where the nerve that was not completely removed was found. Prescribed antibiotics and antihistamines, as the gums are a little swollen. One of the channels is bleeding a bit. They said that if this does not help, then you will have to remove the tooth ((How to be in this situation?
Hello! After complete removal of the "nerve" in the tooth canal put the medicine for a period of 2 to 3 weeks. As a rule, the pain passes during this time, and the channels are filled. The fact that the canal was bleeding is okay, it happens. Without photographs and inspection in this situation, there is no chance to reassure, but if the “nerve” has been completely removed, then everything should be fine.
If the pain reappears and the doctor says that initially there was a big inflammation and that the tooth needs to be removed, then in this case it makes sense to contact another 1-2 specialists to understand the full picture.
He began to respond to the cold and hot lower wisdom tooth. I was put the medicine for 10 days under a temporary seal. Why do not immediately remove the nerve? And one more thing: I put 2 metal crowns on my lower teeth (they couldn’t say cermet - large fillings, they won’t hold). Delivered in February, when chewing, a large amount of food falls in three spaces between the teeth. The doctor said: do not panic, they will sit down. And now it's May, but nothing crouched. Not panic, but terrible discomfort. This is normal?
Hello, Lyudmila! On the first visit, the tooth is opened, the affected dentin is removed and a special medicine is put on the opened nerve, which mummifies the neurovascular bundle in the tooth (kills it), and on the next visit the nerve is completely painlessly removed. Immediately, the “nerve" is not removed due to the high pain of the procedure at the first visit (often the pain is not even stopped by anesthesia).
As for crowns - they must meet certain requirements, one of which is the restoration of the contact point (interdental space). With a correctly made crown that restores the anatomical shape of the tooth, the contact point is restored immediately, and the food should not get stuck between the crowns. The constant ingestion of food between the crowns, leading to discomfort, cannot be considered the norm.
You write that because of large fillings you were denied the installation of cermets - the presence of large fillings is not an absolute contraindication to the manufacture of ceramic-metal crowns. As a rule, cast stump inserts are made that reinforce the tooth and restore its crown part, and then metal-ceramic crowns are fixed on them.
I recommend that you ask for an in-person consultation with another orthopedic dentist - not the one who treated you (or better, in another clinic to get an independent opinion). Tolerate a few more months in the hope that the discomfort will go away by itself is not worth it.
Hello. The doctor put a temporary seal (did not immediately say what kind of medicine) for 5 days. On the third day, all pain disappeared, but he said that it was too early to remove the nerve and that he had put a non-arsenic paste. On the fifth day, unpleasant pain sensations appeared, even with pressure on the tooth with the tongue. The doctor reinserted a temporary filling with another paste (he said that you can walk with it for at least a month) and ordered to call in a week if you don’t get sick. To the question "what if it hurts?" he said he would still call in a week, not earlier - supposedly this nerve wasn’t completely killed, and the pain should go away completely.
Tell me, re-filling for such a period - is this normal? Can't harm a tooth and gum?
Hello, Elena! A temporary filling for a tooth is established if tooth treatment for any reason cannot be made in one visit. As for the presence of a non-arsenic paste in the tooth cavity (to kill the nerve) - such a paste should be in the tooth for at least 7 days, provided that the pulp chamber is partially opened (the cavity where the nerve is located) is opened.
As for arsenic paste, the maximum time for its use is no more than 3 days.
With the correct application of the paste, the tooth should not hurt. Firstly, because the composition of the drug contains anesthetic components. Secondly, necrotization of the nerve contributes to the complete loss of tooth sensitivity. Pain is possible if the concentration of the drug is insufficient, the drug is applied to the closed pulp chamber, as well as in the case of overexposure of the drug.
Given the situation described by you, I would recommend contacting another doctor as soon as possible (who does not consider it normal to go for a week with pain in the tooth in the hope that the pain will still disappear and then treatment can be started).
Good afternoon! Help advice, please. About three years ago, she treated her teeth in a state clinic. One tooth was cured, and the other aroused suspicion. They took a picture - they said that it was necessary to remove the nerve. It came as a surprise to me, because that tooth never hurt and never removed nerves before. Scared. In general, I am very afraid of treating my teeth and it almost always hurts me, even with anesthesia.
About two years ago I gathered my courage and went to a private good clinic to “give up”, because it began to seem that this tooth was a little aching. There she talked about the diagnosis made earlier. They took a picture, checked for sensitivity. They said that the tooth is alive and there is no need to remove any nerve. They just healed caries, and that’s it (to my great joy).
After about a year, it began to seem to me again that the tooth was a little aching. But with a visit to the doctor pulled out of fear ... A couple of weeks ago, still decided and went for a consultation in another good private clinic. They took a 3D image and confirmed that the nerve should be removed.
These all different diagnoses and inaccurate symptoms confused me. Can a tooth with a sick nerve not make itself felt for more than three years? In addition, I am very afraid of all these manipulations. And is nerve removal really necessary? The tooth does not hurt, well, sometimes it seems that it is aching, but it can also be my suspiciousness, or impressionability. Upper tooth)
Hello Olga. Well, I’ll add to your “piggy bank” the opinions of doctors received earlier and my own: judging by your description, there is no need to remove the nerve from the tooth. I would recommend that you see a dentist once every few months so that he monitors the quality of the seal that you have been given in the treatment of caries. You always have time to remove a nerve from a tooth that is practically not disturbing, so there is no need in a hurry. But in the presence of acute intolerable pains with pulpitis that has taken place, or when aching pains completely bother you - the questions and the feasibility of endodontic treatment will disappear by themselves.
Hello! Tell me, please, is it worth it to rush to remove the nerve? Or can you still wait? After treatment, the tooth (four) ached and reacted to the cold. A week later, the whining stopped. Now it hurts to chew and reacts to the cold. The reaction quickly passes after elimination of the irritant. Rarely hears slightly somewhere above the gums, but not for long and not very much. And so for more than a month.
One doctor said that you can wait and watch for symptoms. The second said that it makes no sense to wait, you need to remove the nerve, since the seal is close to the pulp and there is a risk of cyst formation. What to do?
Hello, Tatyana. Based on the symptoms that you described, I would like to agree with a doctor who recommends a tooth depulpation. That is, remove the nerve in the causative tooth. Most likely, at this stage we are already talking about the development of chronic pulpitis, which sooner or later will lead to death of the nerve and infection beyond the tooth. In this case, inflammation occurs in the bone at the apex of the root, and indeed a cyst can form.Therefore, many doctors in such cases recommend not to wait for complications, but to act in advance.
However, keep in mind that in such controversial situations, there are as many doctors as there are doctors. Having received a sufficient amount of opinions and information on this issue, it is important to make an informed decision on your own.
Doctor, tell me what it can be: recently, when I chew in my ears I hear some kind of sound, hollow, as if they were knocking on an empty one. What could it be? My two lower chewing teeth are treated, with the nerves removed. There is no pain, but it gives a decent discomfort, as if eating and it is amplified by a microphone.
Hello Suraye. With this clinical picture, you need to consult an orthopedic surgeon and a maxillofacial surgeon. The orthopedic surgeon should rule out a reduction in occlusion, as this often leads to dysfunction of the temporomandibular joint (TMJ). The surgeon, in turn, will diagnose and prescribe treatment.