Chronic pulpitis may be the outcome of the acute stage of soft tissue inflammation inside the tooth, or an independent disease, but regardless of the cause, it is perhaps the most insidious form of pulpitis. If, with the appearance of acute pains, many quickly seek help, then with chronic pulpitis, most often the symptoms are not expressed, and sometimes the tooth does not hurt at all.
This is where the insidiousness of the disease lies, since the asymptomatic or sluggish course of the disease sooner or later results in, at best, exacerbation of chronic pulpitis with a palette of intolerable pain, and at worst, periodontitis, when it comes to saving a tooth from extraction. Moreover, any attempts to endure periodontitis (as is often done by especially “patient” ones) often lead to suppuration on the roots - cysts, or to complications of periodontitis - periostitis (“fluxes”), osteomyelitis, abscesses, phlegmon or sepsis, when it comes already about saving a person’s life.

How chronic pulpitis develops, what are its characteristic symptoms, features of recognition, treatment, as well as the prevention of complications - let's talk about this later.
What is chronic pulpitis?
Generally speaking, pulpitis is an inflammation of the neurovascular bundle inside the crown of the tooth and root canals. If in acute (focal) pulpitis in certain cases it is possible to stop the inflammatory process and treat the tooth conservatively, that is, without nerve removal, then chronic pulpitis is almost always an irreversible form of the disease. In this case, a gradual degeneration of the pulp takes place inside the tooth: the formation of fibrous tissue, necrosis (necrosis) or the proliferation of the neurovascular bundle until it fills the cavity that leads to the pathology.

According to studies in a number of regions, chronic pulpitis accounts for about 75% of visits, that is, many seek help not because of severe pain symptoms, which often do not occur with this form, but because of the fear of losing a tooth. Typically, chronic pulpitis is the result of an acute form, although children often develop without it. For interesting features of acute purulent pulpitis, see a separate article: Characteristic symptoms of acute purulent pulpitis and methods of its treatment.
Chronic forms of pulpitis are caused by pathogenic microorganisms, as well as their metabolic products, and in most cases the disease is provoked by deep caries or its improper treatment: violation of the tooth processing technique, poor cleaning of the carious cavity, poorly placed filling, etc. Less frequent "triggers" of the development of pathology are:
- tooth injuries
- blockage of canals with stones (salt "plugs")
- penetration of bacteria through the apex of the tooth root in maxillofacial and general diseases (periodontitis, periostitis, osteomyelitis, sinusitis, influenza, etc.)

From the practice of the dentist
Surprisingly, some daredevils are seriously trying to treat pulpitis at home, and they do not even use folk methods for this, but simply barbaric methods for the tooth and body. For example, they take a thin steel needle, heat it red-hot and inject it into a deep carious cavity, thereby trying to cauterize the "nerve" inside the tooth with it. In the best case, by this antediluvian method, the acute stage of inflammation will turn into chronic pulpitis. Quite interesting situations are also when trying"Treatment" of pulpitis with garlic.
By the way, more than 200 years ago, the people came up with a way to extract soft tissue from the tooth canals using an ordinary piano string. The canal itself was then cleaned with the same string.
Symptoms of chronic pulpitis
As already mentioned, chronic pulpitis, unlike acute forms, can be asymptomatic. Acute pulpitis always manifest themselves as very strong paroxysmal pain with small "bright" (not having pain) gaps. All chronic pulpitis is usually characterized by only aching pain at various intervals of periods without pain.
Most often found in dentistry chronic fibrous pulpitis (in almost 70% of cases), less often - gangrenous. Almost never occurs in adults, hypertrophic pulpitis, only sometimes diagnosed at the appointment with a pediatric dentist.


Symptoms of chronic fibrous pulpitis (sometimes called chronic simple) are pain from all types of irritants: cold, hot, sweet, from cold air, etc., which do not go away for a long time after eliminating the irritating factor. Also, this specific pathology is characterized by such a specific symptom as the occurrence of prolonged pain during the transition from cold to a warm room.
On a note
Chronic simple pulpitis, as a diagnosis, is not used by many dentists, since in its name it does not reflect the essence of the degeneration of the structure of the neurovascular bundle. For many practitioners, the question still remains why the author of the Hofung classification calls fibrous pulpitis chronic simple, since in reality this does not reflect the real picture.
Sometimes chronic fibrous pulpitis is asymptomatic. This is due either to the special localization of the carious cavity (for example, under the gum), when stimuli cannot affect it, or to the through message of the cavity and pulp chamber - in such cases there is no swelling and bursting of the pulp, and there are no pains, respectively.
Regarding chronic gangrenous pulpitis, then perhaps the most common symptom of this form of the disease is an unpleasant odor spreading from the tooth. A frequent symptom is also growing pains from the hot, which do not stop for a long time, even after the irritant is no longer in the mouth. Sometimes there are bursting pains in the tooth.
Even if an asymptomatic course is observed, many note a change in tooth color: the appearance of a grayish color. As a rule, the appearance of all these symptoms of chronic gangrenous pulpitis is preceded by acute and spontaneous pains, which then disappear. This suggests that in many people the chronic course of the disease is preceded by its acute form.
In chronic hypertrophic pulpitis, the tooth, as a rule, worries slightly. The main symptom in this case is aching pain when chewing solid food and rarely from temperature irritants. Sometimes bleeding of the tooth during eating is observed, which is associated with the growth into the carious cavity of the pulp of the type of "wild meat" and its mechanical injury. It is this symptom of chronic pulpitis that often scares a person, forcing him to seek help in the end.
Symptoms of rare pulpitis
In the practice of a dentist, pulpitis without caries is sometimes found:
- Traumatic;
- Calculus;
- Retrograde.
Among them, the most common is traumatic pulpitis - an acute inflammatory process that develops against the background of a tooth injury. Acute tooth injury occurs when falling (from a bicycle, from a swing), as a result of hitting various objects (washer, balls), etc. In most cases, the upper front teeth suffer, resulting in severe pain from cold and hot, as well as pain when eating solid food.

If the pulp is damaged during a tooth injury, then the infection joins with the development acute pulpitis pain: prolonged and spontaneous, that is, occurring even without irritants. As a rule, this happens within a day. If you do not consult a doctor during this period, then after some time the acute form of traumatic pulpitis can go into the chronic stage.
Chronic traumatic pulpitis is lethargic, with almost no symptoms. The communication of the opened “nerve” with the environment makes it look like chronic fibrous pulpitis with its characteristic signs. Without treatment, the chronic form can go into exacerbation or periodontitis (inflammation of the tissues around the root of the tooth).
Chronic calculus pulpitis is characterized by slowly increasing symptoms, such as:
- prolonged bouts of pain, sometimes triggered by thermal stimuli (cold, hot);
- long spontaneous pains, sometimes extending to the ear, temple, cheekbone, nape;
- sometimes pain develops when the head is tilted in one direction or another.
This nature of pain is determined by the causes that cause them: squeezing the pulp of the tooth with denticles or petrificates - stone-like formations. Calculi can be detected in the channels of the tooth using an x-ray.
Retrograde pulpitis: has an acute and chronic stage, but differs from classical pulpitis in that it develops without caries. The infection enters the pulp through the apex of the root in diseases such as osteomyelitis, sepsis, sinusitis, etc. In a chronic form, retrograde pulpitis is asymptomatic or with lingering symptoms.

Timely diagnosis and its significance
In order to diagnose chronic pulpitis, in addition to knowing the medical history (complaints, time of occurrence, duration, etc.), the doctor also needs to carry out a set of diagnostic measures.
The most common additional research methods are:
- visual inspection;
- thermometry;
- EDI;
- radiography.
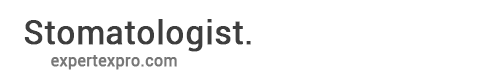
Visual inspection of the tooth with a sharp probe and a mirror gives about 50% of the necessary information. In terms of the appearance of the cavity, soreness of its bottom, communication with the pulp chamber (the place where the "nerve" is), chronic pulpitis can already be assumed.

If there is a message with a carious cavity and pain and bleeding appears when probing with an acute probe, then with a high degree of probability it is chronic fibrous pulpitis. With a change in tooth color, the appearance of a gray tint, with a large amount of softened carious tissue in the tooth cavity, when the “nerve” is partially destroyed and soreness occurs only when probing the canals, it is most likely a chronic gangrenous pulpitis. The appearance of overgrown tissue inside the cavity in combination with soreness when probing it most often indicates chronic hypertrophic pulpitis.
Thermometry. As an additional study, they often resort to thermometry - an analysis of the reaction of a tooth to a cold and, less often, to a hot one. When a tooth reacts to a cold one can safely say that the "nerve" inside it did not die, therefore, we are not talking about periodontitis. For accurate thermometry, you can use special sensors developed by Chepulis and Sirviden, which capture the temperature difference between a healthy and a bad tooth.
EDI or, otherwise, electroodontodiagnosis is one of the most accurate methods for diagnosing pulpitis. Its principle is based on the different electrical excitability of a healthy and diseased pulp.
A healthy “nerve” already reacts with weak pains to a current strength of 2-6 μA. Acute forms of pulpitis react to currents of 20-25 to 35 μA. Chronic fibrous pulpitis is recorded at a current strength of 35-50 μA, with chronic gangrenous - at 60-90 μA.Chronic hypertrophic pulpitis is not diagnosed with EDI, and radiography is used to thin it.
Radiography is a method based on the study of film x-ray photographs of a tooth with surrounding tissues transferred to a computer using an apparatus - a visiograph (unless, of course, we are talking about a modern clinic).

To confirm the diagnosis of chronic hypertrophic pulpitis, the radiograph should not show any changes in the tissues surrounding the tooth and in the area of the interroot septum. In a tooth picture with chronic fibrous pulpitis, most often there are also no changes, but sometimes a slight expansion of the periodontal gap (between the root of the tooth and the socket) is fixed, which complicates the diagnosis. Chronic gangrenous pulpitis is characterized in rare cases by violations of bone tissue in the apex of the roots of the teeth, so the diagnosis is confirmed by thermometry and EDI.
Modern treatment of chronic forms and exacerbations of pulpitis
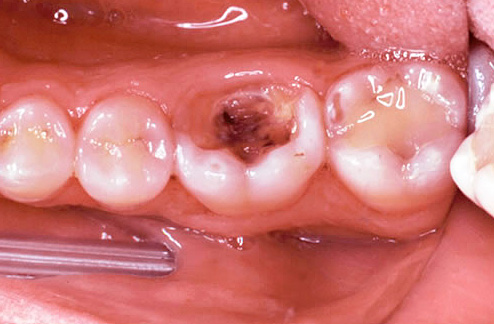
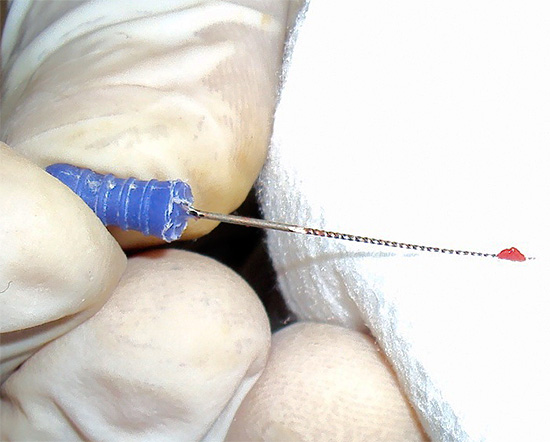
Since chronic pulpitis is an irreversible form of inflammation of the soft tissues, when they can no longer be stored in the tooth, they are most often used for treatment complete pulp extraction from all dental canals. The same approach is followed in the treatment of chronic pulpitis in the acute stage.

In modern dentistry, preference is given to the method of vital (live) extirpation (extraction) of the “nerve”. During the treatment of chronic forms of pulpitis or its exacerbations, only anesthesia is used without additional means for devitalization (killing) of the pulp.
A number of institutions, especially budget ones, still use arsenic paste (“arsenic”) or arsenic-free products for preliminary preparation of pulp for its extraction in the third visit. Anesthesia is also often used, but lack of time, the inability to bring anesthesia to perfection, the rush or the individual characteristics of the jaw of a particular patient lead to the inability to remove the "nerve" immediately.
Arsenic paste is placed on single-rooted teeth for 24 hours, on multi-rooted teeth - for 48 hours. Arsenic-free paste is put on a long term: from 2-3 days to a week or more. Unlike arsenic paste, it does not have a detrimental effect on the tissue surrounding the root, acts slowly and gently. That is why more and more preference is given specifically to arsenic-free products.
From the experience of the dentist
Treatment of tooth canals is a very important event. Removing the “nerves" from the channels here is not enough, as many people think. Only a prolonged washing out of the entire infection from the canal system, treatment of the inner walls of the roots from infected tissues, and then reliable filling can give good results in the long term. If at least one of these stages is violated, then in the near future pain may occur in a “dead” tooth, and changes will begin to occur in the tissues surrounding the root, up to the onset of the formation of a “cyst” - a sac filled with pus and limited by a healthy capsule sections of bone. See also article Tooth cyst removal procedure and its treatment without surgery.
Complications after treatment of chronic pulpitis
After treatment of chronic pulpitis or its exacerbation, patients often feel pains that dentists call post-filling.
On a note
A number of authors are of the opinion that normally such pains should not occur at all, however, the imperfection of the technical and professional component allows minor aching pains immediately after filling (lasts no more than an hour), or pains when biting on a tooth that last from 1 to 3 days.
Post-filling pains that fit into the conditional norm arise due to minor injury to the tissues surrounding the tooth, with a rough separation of the “nerve” during extraction, due to drug treatment of the canal with strong antiseptics, which in small quantities fall outside the root, and also due to the exit of a thin intracanal instrument beyond the apical root opening.

Gross violations of the doctor are:
- poor-quality filling of the channel or channels;
- breaking of the tool in the channel;
- creating perforations in the channel (holes or damage to the root wall).

If in the treatment of chronic pulpitis or its exacerbations there is an incomplete filling of the canals or their excessive filling (removal of material at the apex), then immediately or after a while (from a day to a year or more) there appear symptoms corresponding to periodontitis in the exacerbation. In this case, there may often be acute pains, the inability to touch the tooth even with the tongue, the pulsating nature of the pain, and in some cases, after some time, swelling of the mucous membrane in the region of the apex of the root of the tooth may occur.
When a tool breaks off in the canal, the tooth may not manifest itself for a long time, but sooner or later the infection in the “uncleaned” and not sealed root section will cause either a purulent process in the canal with the formation of a “flux”, or the process will have a chronic form with formation at best fistulas (ducts that open on the gums, through which pus from the root of the tooth is secreted into the oral cavity), and in the worst case, the formation of purulent sacs - cysts.
Perforation, or, in other words, a “hole” in the root, manifests itself almost always immediately. Often the patient himself notices when the doctor mistakenly left instead of the canal into the “gum”. As a rule, a few hours after such treatment of chronic pulpitis or exacerbation, severe aching pains or acute paroxysmal pains occur. Sometimes even painkillers may not help.
To summarize ...
At the first symptoms of chronic pulpitis or its exacerbation, you should immediately consult a doctor. To give a 100% guarantee that during treatment there will be no complication, not a single clinic can, but in many of them there is a special approach to the treatment of chronic and other pulpitis, which makes these risks minimal.
So, for example, many expensive dental clinics pay much attention to the intracanal treatment of chronic pulpitis, devoting at least 1 hour to this procedure (for a single-channel tooth). Budget organizations cannot boast of such a reserve of time for the mechanical and drug treatment of channels and their filling alone. But any rush increases the risk of complications ...
The leading role in the prevention of complications is played by the professional training of the dentist and the level of equipment of the clinic. Therefore, it is important to obtain maximum information from relatives and friends about the clinic and its doctors before treatment. The correct choice of the institution and the doctor will allow you to successfully treat and seal the canals, preserving the tooth for many years.
An interesting video about the causes of pulpitis and its potential danger
An exciting example of removing a broken instrument from a tooth canal