
When it is not possible to save a sick tooth (or simply a problem one), dental surgeons come to the rescue to remove it, trying to save a person from the corresponding pathology and health risks. However, it also happens that after the tooth extraction procedure, the resulting hole does not heal for a long time and begins to hurt, and the suffering can intensify every day. In these cases, they speak of complications after tooth extraction, the various types of which we will consider later.
Unfortunately, some people relate to problems that occur after tooth extraction, without proper attention - they say, it's okay, it will hurt and stop. Sometimes even obvious symptoms are ignored, which in some cases may well become fatal for a person, for example, prolonged bleeding from a hole, putrid breath from the mouth, swelling of tissues adjacent to the hole, and some others. You can’t do this!
It must be understood that the removal of any tooth (especially the wisdom tooth) is not just ordinary dental manipulation, but an operation that involves the creation of an artificial wound, bleeding and traumatic inflammation of the soft tissues around the hole. As with other operations, there are always risks of developing postoperative complications, which in this case, when suppuration of the hole can lead to such serious complications as, for example, an abscess, osteomyelitis of the jaw, phlegmon.
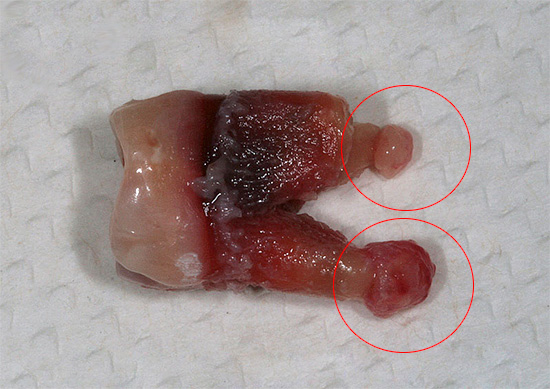
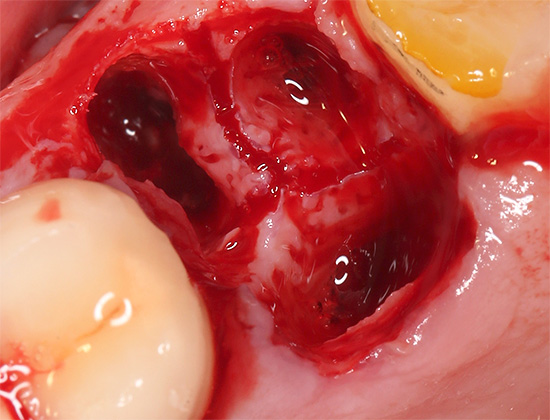
In the photo - the consequences of osteomyelitis of the jaw:

This is interesting: why does the pain occur after tooth extraction?
The first source of pain is injured tissue over the entire area of the dental socket - the nerve endings located here are irritated, causing pain. However, as the hole is filled with a blood clot, soreness often disappears, as a kind of biological defense appears. The second source of pain is the periosteum - a film of tissue surrounding the jaw bone on the outside. If it is disturbed during anesthesia and / or after tooth extraction, a hematoma can develop under it, which also causes pain. The third source of pain is edema inside the jaw bone, which sometimes forms, for example, after traumatic removal.
If wisdom teeth are difficult to erupt (pericoronitis), an incision is made in the gum before they are removed, as a result of which it is also traumatized, it may hurt in the future and may even require some treatment.
Loss of consciousness after tooth extraction
After tooth extraction, a fairly common complication may occur, such as fainting or short-term loss of consciousness of the patient as a result of intense psycho-emotional stress or stress. It occurs against the background of a deterioration in the supply of oxygen to the brain.

Temporary loss of consciousness is a common complication that, generally speaking, can develop both before and after the removal procedure. Moreover, as practice shows, even if you are a man who is not afraid of the sight of blood, this does not guarantee that during, for example, a difficult removal of a wisdom tooth, you will not lose consciousness.
Due to the fact that during the tooth extraction surgery, the dentist-surgeon may not act professionally enough, apply imperfect working techniques, allow inaccuracies and errors, and in some cases even rudeness and incorrect behavior in relation to the patient’s personality, in such cases, significantly increase risks of fainting after undergoing a procedure.

If, during treatment, the doctor adheres to the principle of an individual approach to his patient, takes care of his health, is neat and polite with him, then the risk of loss of consciousness at the dental appointment is minimal.However, even in such cases, people who were frightened by the Soviet barbaric methods of removing tooth roots with a chisel and hammer, still sometimes cannot overcome an insurmountable fear during surgery, which can result in such a general complication as fainting - even against the background beautifully performed manipulation.

To restore consciousness to a person, the dentist carries out a simple algorithm of actions:
- Moves the patient to a horizontal position;
- Provides an influx of fresh air;
- Relaxes tight clothing;
- Sprays face with cold water;
- Allows you to inhale vapors of ammonia.
After inhaling ammonia, consciousness usually returns in a matter of seconds.
From the interview with the dentist
I have been working in surgery for more than 15 years, and over the years of my working days in hospitals and clinics I have seen many interesting cases of fainting. Loss of consciousness can occur before or after tooth extraction, it can be foreseen, or it can be overlooked. From the most unusual fainting, I can cite a number of examples.
One guy (19 years old) literally 5 seconds before passing out said a phrase addressed to me: "Now, doctor, I’ll disconnect." Then he lost consciousness.
In different years, there were two cases when, before the blackout, two young children had a “shaking" of the body for 5-10 seconds (convulsive fainting), after which the convulsions stopped. Moreover, there was no history of seizures or epilepsy, and consciousness returned after a minute under the influence of ammonia.
In my practice, there was also a case when a woman sharply got up from a chair after tooth extraction and fainted, hitting the doctor’s table and breaking the glass on it. By a happy coincidence, there were no serious injuries.
The main thing is that fainting is a short-term loss of consciousness, so neither young beginner doctors, nor too emotional and impressionable patients should be especially frightened of this general complication, but you should always be prepared for this.
Dentist-surgeon Stanislav Gennadevich, Perm

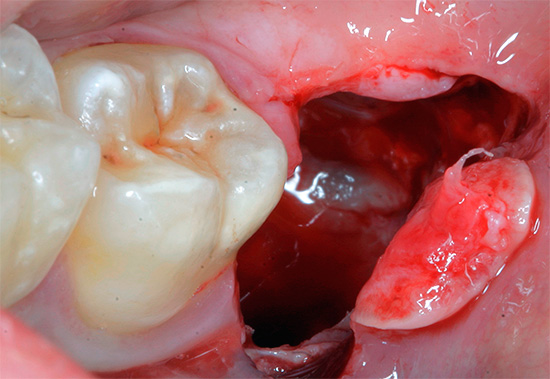
Local complications arising after tooth extraction
After tooth extraction, certain local problems or local complications may occur. The following complications after tooth extraction are the most common at the surgeon’s appointment:
- Holey bleeding;
- Incomplete tooth extraction;
- Alveolitis after tooth extraction;
- Paresthesia (loss of sensitivity).
It is interesting
The most common complication after removing a wisdom tooth is an increase in body temperature on the day of removal, sometimes to high numbers (up to 38.0 degrees). If removal was difficult, the tissue around the wound may be inflamed and swollen.
It is inflammation without the addition of a purulent infection, as a reaction to an injury in the mouth, that causes an increase in temperature, so the detection of such an manifestation of the body on the first day after the removal of a wisdom tooth is almost always not a complication. If you maintain a high temperature on the second and third day, as well as other symptoms of possible complications (for example, putrid odor, severe pain), you should consult a doctor for advice.
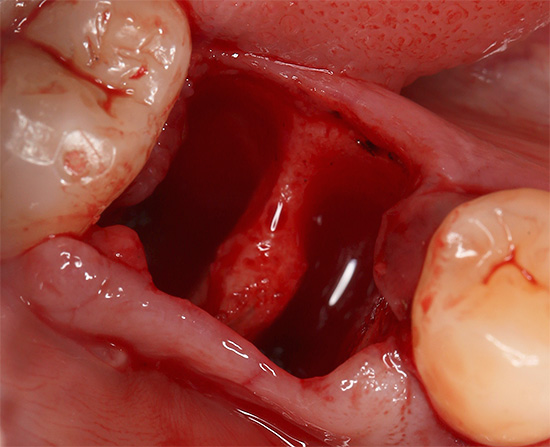
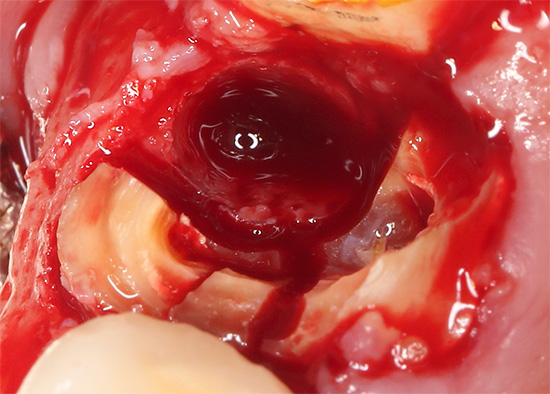
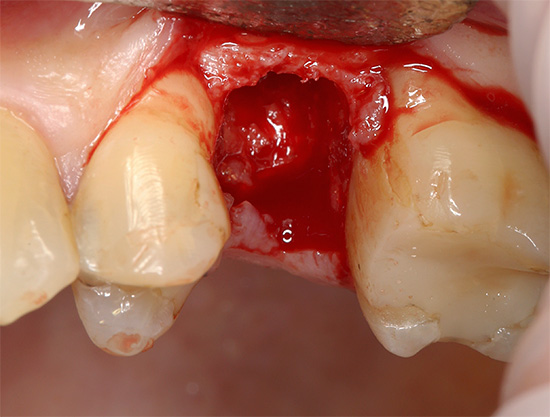
Hole bleeding
Hole bleeding can develop immediately after tooth extraction, or maybe delayed - after a few hours or even later. It occurs when damage to the small vascular network in the tissues, and refers to local complications after tooth extraction. A blood clot serves as a biological defense, so much depends on its proper formation.
Blood in the well should normally stop for a short period of time, on average - 5-15 minutes. In principle, a slightly bleeding hole for several hours is also not a problem after tooth extraction. Such wells sometimes heal even faster than with a quick stop in the blood.Another thing is if after removal there is severe bleeding that cannot be stopped by anything.
The most risky option is to stop the bleeding without understanding its causes. Drugs for stop bleeding after tooth extraction it can be administered intravenously (aminocaproic acid) or intramuscularly (Vikasol), localized products such as a hemostatic sponge or gauze swab over a wound saturated with 3% hydrogen peroxide can be put into the hole of a removed tooth. But without determining the true cause of the bleeding, all of these treatment procedures may simply be useless.
Possible true causes of bleeding from the hole:
- Diseases associated with impaired blood coagulation, or with damage to the vascular system of the blood (hemophilia, C-vitamin deficiency, acute leukemia, scarlet fever, hemorrhagic vasculitis, infectious hepatitis, etc.).
- Arterial hypertension (high blood pressure).
- Concomitant treatment with anticoagulants of indirect action, otherwise - with drugs that "dilute" the blood.
- Increased blood sugar in diabetes.
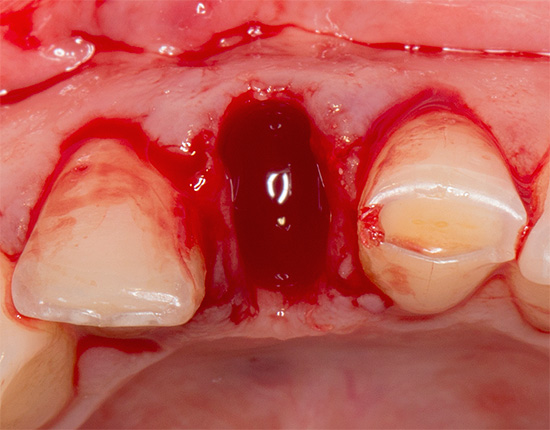
Such a complication after tooth extraction, such as severe and prolonged bleeding from the hole, can lead to a deterioration in the general condition of a person, the appearance of weakness, dizziness, pallor, and a decrease in pressure. Most often, such complications develop after roughly performed extraction of the lower wisdom tooth, since it is in the region of the 8th tooth that most of all are soft and well-supplied with blood tissues. Especially traumatic can be the so-called complex removal of the 8 tooth, when it has to be taken out of the jaw literally in pieces.
Incomplete tooth extraction
In most cases, such a complication as incomplete tooth extraction occurs only when the inexperienced or not responsible dentist surgeon performs the procedure (do not think that this is an incredible rarity - such a doctor can also be found in a respectable dental clinic).
When a tooth is extracted from the hole together with the roots, or each root separately, an important aspect of the doctor’s good work is to check the extracted object for breaking or breaking off a piece of the root. If the doctor does not check the tooth after extraction, or deliberately keeps silent about the problem of breaking off a part of the root in the tooth socket, and tells the patient that everything is normal, then after the removal, in addition to long-term pains, serious complications can occur (suppuration of the gums, and in severe cases and without treatment - an abscess, up to jaw osteomyelitis).
It is interesting
After leaving part of the root in the hole, another scenario is possible. After such a serious mistake on the part of the doctor, the hole may even begin to heal normally, and sometimes it is almost painless. If there was “inflammation” at the top of the left root in the form of a discharge of bone tissue or granuloma, or a tooth cyst (purulent sac), then over time the process will only worsen, provoking the development of infection in the area of this limited area.
It may take years before a granuloma or cyst “shoots” and a person gets such a complication as periostitis (flux), abscess, or phlegmon, but access to the root left in the hole will already be blocked by the gum from above, so an urgent operation with a gum cut will be required.
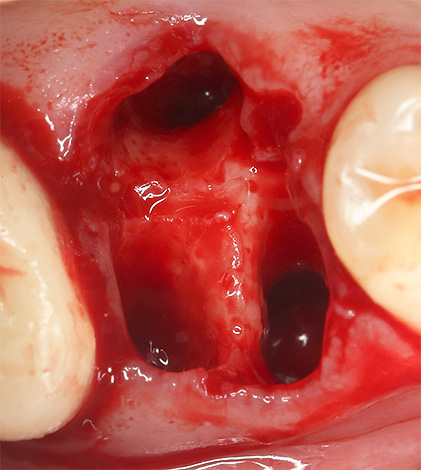
Alveolitis
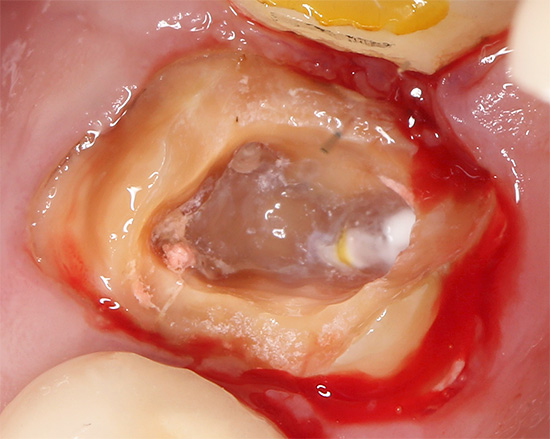
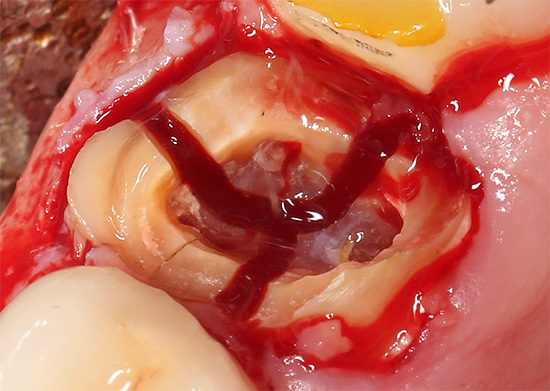
Normal healing of the hole after tooth extraction starts the process of replacing a blood clot with granulation tissue, which ultimately leads to the formation of osteoid tissue - young bone. If, after tooth extraction, a blood clot did not form and an infection got into the hole, or, for example, there was a traumatic removal of a wisdom tooth with large breaks in tissues, then inflammation (suppuration) of the walls of the hole - alveolitis occurs, which leads to pain and swelling of the gums.
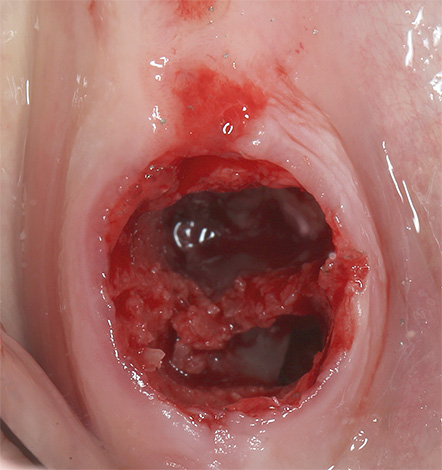
Often, a putrid odor from the mouth appears, purulent discharge from the hole is observed: it is covered with a gray coating, it almost always does not have a blood clot or is damaged, and a general inflammatory syndrome with symptoms of intoxication of the body often develops. Due to alveolitis and related purulent-necrotic processes, they can become inflamed, become painful when touched, and the lymph nodes grow in size.
Without proper treatment, a transition of alveolitis to limited osteomyelitis of the jaw may be observed - a serious complication that occurs most often after careless removal of a large molar (for example, a wisdom tooth).

Paresthesia after tooth extraction (loss of sensitivity of the tongue, lips, areas of the face)
Most often, this complication manifests itself after the removal of a wisdom tooth, and almost always through the fault of the doctor. In trauma to the deep layers of the bone, there are risks of damage to closely passing nerves (lingual and lower alveolar nerve), which causes numbness of the tongue, lips, chin and cheek, which does not go away for a long time.

With minor damage, sensitivity is restored on average in 1-2 weeks. In more severe cases, treatment may require the help of a maxillofacial surgeon together with a neurologist.
Recommendations after tooth extraction for the prevention of severe consequences
In order for the well to heal after tooth extraction without serious complications associated with the attachment of a secondary infection, it is useful to adhere to a number of rules that make life easier after surgery and reduce postoperative risks.
In order to feel as comfortable as possible after visiting a dental surgeon, you must:
- Remove the gauze swab 20 minutes after tooth extraction.
- About 3 hours do not eat.
- Apply a cold compress to the area of operation and repeat this action every 2 hours for 20 minutes (during the day after the intervention).
- Three days do not eat hot, rough and spicy foods.
- For 2-3 days, eliminate serious physical exertion, do not take a hot shower, do not visit the bathhouse, sauna, solarium. Refuse sports. Protect yourself from overheating and hypothermia.
- Do not rinse the wound after tooth extraction. It is better to do oral baths: put an antiseptic in your mouth - spit it out. For oral baths, it is optimal to choose decoctions of sage or chamomile.
- Avoid hard foods, chew the first days after removal by the other side of the jaw.
- Use a soft toothbrush for 5-7 days, while maintaining particular care.
- Follow the doctor’s prescription: if the dentist-surgeon prescribed antibiotics in a 7-day course, then you can’t stop taking it, because after such a break, this antibiotic may no longer work, because for a short use of the drug, microbes often have resistance to it.
Long-term effects of tooth extraction
Alveolitis, abscess, osteomyelitis of the jaw, sometimes even sinusitis - these are complications after tooth extraction that may well occur if you do not pay due attention to the corresponding symptoms in time. Meanwhile, almost anyone can recognize the corresponding threat and prevent serious consequences - for this it is enough to be guided by at least common sense and not be afraid to consult a doctor again.
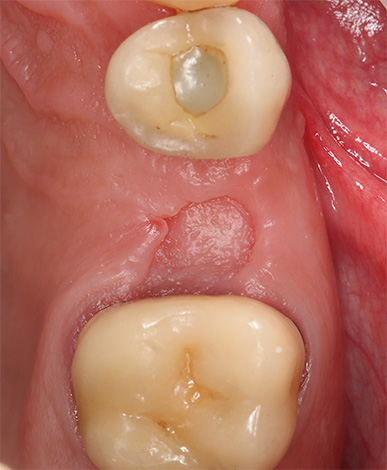
However, common sense often does not work in cases where the hole heals normally and everything seems to be fine: most people, rejoicing at the normal healing of the hole for 2-3 months, forget that the pale pink smooth gum in place of the former patient tooth is not an indicator of quality of life in the future.

Simply put: tooth extraction requires replacing it with an artificial structure. It can be any crown, removable or bridge. In the end, no one forbids putting the implant in place of the extracted tooth, and then the crown or bridge, if the defect is long.
Inaction and expectation of problems are very destructive, and sooner or later they come to every second owner of different-sized gaps between the teeth. First of all, I would like to say about the most desperate and careless citizens who continue to bite and chew with their front teeth for years in the absence of all or most of the chewing teeth, and at the same time each time they complain that the fillings somehow fall out quickly or the teeth are loose or erased. It comes to the fact that the search for the truth leads such a patient to the doctor again and again, until the seal established 10-15 times again breaks off, falls out, or until the tooth is erased to the level of the gums or loosened and removed by “hands”.
Patients in search of the truth can go very far, but sometimes they can’t understand basic things. After all, the dentition is an integral and interconnected system. With the loss of a tooth, a natural displacement of adjacent teeth occurs in the direction of the appeared gap. As a result, from the patient you can hear something like “the teeth went” or “the bite was broken.” And this, generally speaking, is also a kind of complication that often occurs after tooth extraction, if you do not take appropriate action.

And how does the tooth that has lost its “colleague” below or above suffer! If he loses his antagonist from the opposite side of the jaw, then the load does not go on him, which means that the body considers him superfluous or foreign. Therefore, a person notes how a tooth begins, as if, to gradually grow in the jaw, but in fact - it is put forward, with a high risk in the future to "leave" the jaw. And this is only half of what can happen without prosthetics.
If we touch on the problem of clicking and cracking the joint of the lower jaw, then the common cause of its deformations and disorders will surprise many: the condition of the temporomandibular joint directly depends on the state of the bite. It is impossible not to say that with violations in this joint, hearing loss may even occur. That is why it is so important to replace the removed tooth with an artificial structure as soon as possible.
Inflammation of the hole after tooth extraction: what can you expect in this case in the dentist's office
What to do immediately after tooth extraction to prevent complications



Good afternoon. Please tell me what I have. A month ago, the retiniated lower eight was removed. Today, during a meal on the opposite side, a crack occurred suddenly in the place where the tooth was removed, as if the jaw had broken, with wild pain, and now the removal site hurts, I can neither eat nor open my mouth wide. During a conversation and when I am silent, the pain is aching, but not strong. I can’t bite anything, the feeling that the jaw is apart. When feeling, there are no discrepancies, of course, no ... But what happened, I do not understand. What could break with such a crunch? Ahead of the weekend ... How to be - I can not imagine.
I will add: I was at the dentist in the morning, we took a panoramic picture, the doctor does not see any cracks and a fracture (it pleases).But now it hurts me when I bend my face down, the feeling that some kind of heaviness is pouring into this place, and I can’t chew even on the opposite side - the feeling that the jaw is apart. The real feeling is that something has broken off there. The doctor did not give any recommendations, said, be patient, it should pass. What happened and what to do?
Hello! So it’s difficult to assume something right away; in such a situation, inspection and pictures are important. First of all, I would like to exclude subluxation of the joint of the lower jaw. Maybe during the meal there was a moment when he shifted with a crunch. The fact is that during removal, there could be an excessive opening of the mouth + your existing joint deformations, which sometimes take years to form. Here you need to know exactly whether there was pain in the ear area, a crunch in the joint, knocking, etc. Basically, nothing else comes to mind. Not sure if the doctor could leave the sharp edges of the bone or something foreign. It would be nice to show a picture of the hole not to the attending physician, but to another dentist with an independent opinion. If there is a suspicion of a joint, images of the TMJ for deformation will help. Thanks for the question.
Good afternoon. Turned to the ChLH, made a three-dimensional picture, a crack in the region of the angle of the lower jaw. They recommended a tight dressing for 2 weeks, calcium and mummy preparations, a Dimexide compress for the night, and nutrition for 6 months with grated and liquid foods without chewing. In addition, the image showed that, as a result of the removal, the walls of the well were very thinned. The operation was carried out by drilling. The doctor at ChLH said not to strain his jaw and eat only grated food due to the fact that a fracture is possible before the formation of hard bone tissue in the hole from the extracted tooth. What else do you recommend? The fact is that in the next 3 weeks a gynecology operation is planned under general anesthesia, I'm afraid that serious injury can really happen when I open my mouth for the purpose of anesthesia and insert a breathing tube (or as it is called, sorry, I don’t know for sure). What do you advise? Warn the anesthetist about possible injury?
I add, tooth extraction was in another country, so the surgeons in my city are independent in this situation.
Hello! Now the causal relationship has cleared up a bit. I think that the excessive destruction of the alveolar process in the region of the angle of the lower jaw, or the excessive “persistence” and carelessness of the surgeon provoked a crack. This, of course, is a serious complication after tooth extraction. I think that an anesthesiologist’s warning here is indispensable. If the gynecological operation is planned, then it is better to transfer it with supporting certificates (documents) that you have a number of nuances that make it difficult to anesthetize, and in general - the fact of an injury + an unhealed hole after removal complicates the situation for the future gynecological treatment. If you cannot postpone for certain reasons, it is important to get advice from a future anesthetist + operating gynecologist, so that later you and your doctors will have no problems. Thanks for the question.
Thank you very much for your help in making a decision and giving advice. There is no way to transfer the operation. I will talk with the surgeon and anesthetist, as you advise.
Removed 8-ku (48 tooth), 3 days ago. They put 3 sutures on the mucosa, as there was a large wound (the tooth was located at an angle of 90 degrees to the gum). The seams today parted, a huge wound. What to do?!
Hello! Urgently consult a doctor, since the sutures are applied largely so that the wound does not represent a reservoir for infection from the oral cavity.I think that the doctor will find an opportunity to help you: if there is a need, then the sutures will be re-applied, but no - then you will safely be treated at home according to the adjusted list of recommendations.
Hello! Removed 5 root (left top). From the bottom left, the dead eight, also to be removed, began to climb out of the gums, as well as the dead 4, also got out (almost sure) next to the 5-root removed three days ago.
Due to the rise of the eight, the bite has changed. And as far as 4 came out - I can’t check. What is the reason and how to put 4-ku in place? It is planned to build a bridge in a month, when the gums heal. The doctor has not been. Thanks.
Hello! Unfortunately, it’s hard for me to understand the essence of the problem from your description. What 4 - it’s not clear what you are describing. If you want, you can clarify, as well as send a panoramic picture, I will look and comment on it.
Tell me, please: the tooth was removed, the lower jaw, the gum becomes inflamed, periodically swells, then passes. I went to the doctor - cut the gum, cleaned. What infection could bring?
Hello! I think that it was said not quite correctly: most likely, this is not about infection by a dentist. The fact is that you are faced with alveolitis - inflammation of the hole. This sometimes happens if the dentist badly cleaned the hole from foreign components (parts of the tooth, roots, granulomas, cysts, etc.), and also often when the patient does not follow the recommendations, even if the doctor did everything correctly. If the hole after removal turns into a kind of storage of bacteria and food from the oral cavity, then its healing can be significantly complicated by the attachment of an infection. The only question is what kind of immune response should be expected in a particular case, and he (this answer) is always individual. The fact that they helped you in your situation is good, but I have no idea what mistakes the dentist-surgeon made initially, and whether there were any mistakes, because normal healing of the hole (without attaching the infection to the wound) is the result of a full interaction of the doctor and actions of the patient in the postoperative period.
Today removed the bottom retained figure eight. Spent an hour. They made 5 injections. They cut the gum and then picked it up with something - it feels like they are picking out a seal. They pulled a stick. Drilled, pulled again. And all, got a whole tooth. They cleaned the wound, put a clot (it was made from my blood from a vein), 4 sutures. Then they gave ice, kept it for about 20 minutes, then home. The cheek is a little swollen, it hurts to swallow. When the anesthesia was gone, I took it. Now it doesn’t hurt much, only when swallowing.
In general, deleting is not painful. It hurts when the anesthesia goes away. But very scary. I, while being pulled out, my legs were shaking and sweat was already dripping from my ears)) But now I understand that there was nothing to be afraid of. While removed, you do not feel pain at all, only unpleasantly. It hurts then, at home.
Five days ago, teeth were removed on the lower jaw, bone grafting was done. After removal of the lower four, there is still no sensitivity of the lip!
Hello, my wisdom teeth come out from above and below, at the same time. The bottom almost completely broke through, left a little from the end of the gum, which rises to the touch (I don’t know for sure, it seems to be called the hood). And the upper tooth on the same side grows crookedly and presses on the other teeth, the gum is swollen, any touch causes pain. The whole mouth was inflamed, a lot of stomatitis appeared in the mouth, I can hardly eat. The temperature rises to 38.5, the lymph nodes are swollen. But the worst thing is that my mouth does not open wide due to TMJ dysfunction, which has been present for more than 3 years. The mouth does not open fully to even yawn.I also can’t tolerate the pain of a wisdom tooth. Tell me, is tooth extraction realistic with such a diagnosis?
Hello! You describe those symptoms that determine the indications for urgent removal of the wisdom tooth (s) (if there are no contraindications requiring special conditions for removal - for example, from the side of the heart). As for the possibility of tooth extraction from outpatients: unfortunately, I don’t see how “small” your mouth is. The fact is that I personally came across cases where the patient says that removing the wisdom tooth will not work, because the mouth does not open well, and I removed it without problems, since there were really no serious obstacles to this. However, I cannot underestimate your complaints - if you say that your mouth does not open well, then suddenly, in fact, everything is very bad in this regard ...
An ideal option in order not to lose time is maxillofacial surgery with its own hospital. There, specialists are able to do anesthesia using the extraoral method, which is almost always inaccessible to dental surgeons in hospitals and clinics. And this means that your case will not cause trouble for experienced doctors and everything will go as well as possible. Moreover, you already have a TMJ pathology, which is just being treated in a specialized institution by maxillofacial surgeons: according to the diagnosis, surgical (if necessary) treatment options are planned, or physiotherapeutic ones with occlusion correction according to the samples.
So I tell you “from my bell tower” that the extraction of such teeth is quite real. However, if you want to remove your teeth as safely as possible and taking into account the concomitant pathology - now you know where to do it.
Hello! Please help with the answer. On Saturday, a tooth was removed, 6-ku, on the left side. There is numbness of the lower lip on the same left side, the lymph node is slightly inflamed. A gray film appeared in and around the hole.
Hello! Judging by the description, there is a risk of developing alveolitis + as a result of traumatically performed manipulations, paresthesia (numbness) occurred. Inflammation of the lymph node may indicate a background infection, or a response of the body to tooth extraction and the onset of purulent infection in the hole. I am sure that it is urgent to contact the dentist to assess the situation. It may be necessary to take a snapshot of the deletion area to outline an action plan to eliminate this problem. Thanks for the question.
On February 17, my lower wisdom teeth were removed from my daughter (on the recommendation of the orthodontist). They drank the prescribed course of amoxiclav (7 days). On March 6, a swelling appeared in the region of the angle of the lower jaw on the left, 7 intensified. We went to a surgeon in the ChL - they prescribed a new course of amoxiclav for 7 days (875 mg 3 times a day). The swelling of the soft tissues has decreased significantly, but with pressure on the gum, pus comes out. Yesterday, the surgeon washed the gums and told him to continue drinking amoxiclav. How many days can you drink an antibiotic as much as possible?
Hello! 2.5 weeks after the removal of the lower wisdom tooth, a purulent process arose? To put it mildly, it’s strange if everything is as you say. In addition to taking an antibiotic, you must definitely try to find out why this is happening. The reason may be anything: a neglected alveolitis, an infection in a tooth adjacent to the extracted tooth, not removed tooth roots (or root), fragments, granulomas, cysts left in the hole, etc. You say that the removal was planned, but nothing can be denied, since the situation is not typical. All the most unpleasant (acute symptoms, swelling, fever, etc.) was supposed to happen in the first 3-5, maximum 7-10 days after removal, and then 2.5 weeks: from February 17 to March 6. Strange situation.
And about the antibiotic Amoxiclav - up to 2 weeks, depending on the severity of the situation and the available indications for admission.
Hello! Thanks for the answer. The fact is that we are now in Spain. After tooth extraction there was a flight on an airplane, a climate change. Before taking PMF, a picture of the jaw was taken - no bone pathology was detected. Amoxiclav drank 2 weeks. When pressing on the seam area, pus is released. The surgeon recorded an operation, but after 1-2 weeks. He said if swelling appears again, drink levofloxacin 500 mg 2 times a day. But the child is 15 years old, and in the annotation it is written that it is impossible to 18 years. I do not know what to do…
Hello! Without seeing the clinical picture firsthand, it is difficult to say what allowed the doctor to back off the instructions and prescribe this antibiotic. Be that as it may, pus should not be there for a long time. It is important to find out why such a deviation from the norm occurs; the health of the child is at stake. I would advise getting face-to-face consultations with several doctors. I know many cases when other doctors could find gross errors of the first dentist who persistently insisted on the impeccability of his approach to treatment. It makes no sense to pull.
Hello! Tell me please. A week ago, she removed a wisdom tooth in her lower jaw. Removal was difficult. The first 2 days the wound was bleeding, but the temperature was up to 37. By 3-4 it rose to 38. After removal of the cheek, the swelling in the upper part, slept two days later, but the swelling went below the cheek (albeit small). As such, there is no severe pain, but occasionally breaking through, throbbing! It is still painful to swallow and open your mouth after a week. The surgeon turned out to be a complete boor! I don’t want to ask him. Tell me what to do next?
Hello! In this situation, it is better to contact another dentist surgeon, since the symptoms you described are worrying: swelling, difficulty opening the mouth, temperature, etc. The fact that the doctor, as you write, is “boorish,” can also determine the possible leaving in the hole of fragments of a tooth, granulomas, cysts, etc. I would advise you to take a picture of the hole as a diagnostic in order to know for sure whether the doctor made serious mistakes or not. Most likely, a hole curettage will be needed: due to this, the wound heals as quickly and comfortably as possible. So I advise you to quickly find a good doctor, consult with him (in person) and, possibly, correct the mistakes of the previous doctor.
Hello. Tell me please. 2 weeks ago, the chewing tooth was removed below. A week later, she came with pain, washed, prescribed tsifran (since penicillin is allergic) and nise, drank. So, 2 weeks have passed, the hole is delayed. I look around, and there a white-yellow coating, and twitches a little, but not much. Is it worth the alarm? Thank you very much for the answer.
Hello! I think it’s not worth the alarm. White-yellow plaque - a condition within normal limits. When chewing food, the gums may bother until the hole is fully tightened. 2 weeks is a decent time for the situation to normalize. All the risks have long been behind, there are no serious symptoms, that is, it’s definitely not worth worrying about the plaque and some soreness of the gums. For more comfort and with a strong desire, you can do a control examination of the hole at the dentist: the doctor will definitely not be offended, and your cats will stop scratching your soul.
Tell me please. Deleted 8, after 3 weeks there was sensitivity to cold and mild pain, especially after drinking cool water in the place where it was 8.
Hello! Apparently, in this case you are worried about the 7th tooth, the distal wall of which turned out to be with an open cervical area due to gum “subsidence” (there may be cervical caries). This problem is best investigated directly in the dentist's chair in order to accurately determine the cause.
There is also usual hypersensitivity due to gum injury after removing a wisdom tooth - it takes about 1-2 weeks on average, but you say that you have it after 3 weeks, which no longer fits the norm.So it’s worth checking the 7th tooth for caries. The sooner you start treatment, the more likely you are to keep the tooth alive without removing the “nerve”. Good luck
Tell me please. In December, she removed the lower eight; after removal, the jaw opened 1 cm for 2 weeks. The surgeon prescribed an MRI. MRI showed that everything is fine. Now the jaw hurts, crunches, the mouth does not open in full. What is it?
Hello! If you mean that MRI was used to diagnose TMJ, then in your case it’s unlikely that “everything is fine.” There is definitely a problem in the mandibular joint: a certain degree of deformation, a change in position or a “loosening” of the ligamentous apparatus. Six months after the removal of the wisdom tooth, there should be no normal manifestations.
In the event that the diagnosis of the joint or joints on both sides has not been carried out, be sure to conduct and get advice from the maxillofacial surgeon. If the doctor can’t see anything from the pictures taken, then contact other specialists. I think that a crunch and a violation of the opening of the mouth are caused precisely by a problem with the temporomandibular joint.
Hello! 4 days ago, the lower chewing tooth was removed, the procedure was a bit complicated, as the tooth crown broke off and it was necessary to remove the tooth in parts. There was a slight inflammation at the root of the tooth, but I did not feel it before the procedure. After the procedure, the doctor pulled out a tooth with the root. The wall of the dimple, on the cheek side, is slightly torn. There was very little blood in the hole, but still a clot formed. The day after the removal, the cheek swelled, the temperature rose to 37.4, the aching and very unpleasant pain tormented. On day 3, the temperature was already falling and did not increase anymore, but the hole was a little bloody, still sick on day 4. The hole is covered with a grayish-red coating. I open my jaw calmly, it does not cause trouble. The edema seemed to be sleeping a little, but quite a bit, the pain remained. I drink painkillers, no bad breath. Is all of the above normal?
The wound was healed, but it hurts, and the swelling bothers. How can I alleviate the condition?
Hello! According to your description, some fears are caused only by the grayish color of the clot and persistent swelling of the gums. However, in the absence of other symptoms (fever, significant swelling, severe pain, putrid breath, etc.), it is hardly possible to talk about alveolitis. So I recommend that you strictly follow the doctor’s instructions, and get 1-2 consultations with him during the healing of the hole to remove all doubts. It would be wrong to recommend you any preparations or procedures without a personal inspection, as it is fraught with complications.
Hello. He removed the 6th tooth. A white cloth appeared in place of the tooth (I can’t find the word, something like a white gauze in appearance). It doesn’t hurt much, a slight pain of adjacent teeth. I want to clarify, is this not dangerous?
Hello! A whitish or yellowish plaque in the hole (on a blood clot) is not a pathology and often accompanies the healing process of a wound after tooth extraction. The pain of neighboring teeth in such cases is caused by a gum injury - this is temporary, the pain will decrease every day as the damaged tissues recover. Pain disappears on average in 5-14 days. Follow the recommendations of your doctor and be healthy!
Please tell me, is it possible to take hot injections on the day of tooth extraction?
Hello! I would not recommend any procedures on the day of tooth extraction without urgent need.As a last resort, you need to consult a general practitioner who treats your underlying condition to weigh the risks. During and after tooth extraction, the load on the body increases, and parallel intervention in its work at this time is not always advisable.
The septum of the lower jaw is visible, removal was difficult. The hole has not been closed for a month now, what should I do?
Hello! I recommend that you correct the septum under anesthesia as soon as possible. It is not long, but it will provide comfortable conditions for healing. Moreover, you write about the difficult formation of the gums, although a month has passed since the extraction of the tooth. See your maxillofacial surgeon for an appointment and freshen the wound (suturing may be necessary).
Hello! Please advise me how to be. 4 days ago, removed the wisdom tooth on the lower jaw. On the second day, it became difficult to swallow. Thought it was a sore throat. On day 3, it began to swell: gums, gland, and the entire larynx. Outside is a swelling of the lymph node. I swallow with very great difficulty and pain. Mouth, one might say, does not open. Temperature 35.8.
Hello! Urgently seek maxillofacial surgery where there is a hospital. Hospitalization may be required. According to your description, these are formidable symptoms, dangerous because tooth extraction could not bring results, and the infection has already moved along the maxillofacial spaces, creating risks of sepsis and mediastinitis. Do not blame the doctor who removed the tooth, and, especially, spend time on conflicts - immediately run for help.
Hello, 10 days ago I removed 2 teeth - 8. One upper and one lower, both on the same side. On the other hand, 8 is also removed, but much earlier. There is an upper 7 tooth and a lower 6, which are cut down to cermet on the same day. Wells are tightened; sutures were applied after surgery. There was no temperature, the cheek had a swelling in the first days. I felt great, then I felt a slight smack of pus, went for a wash with Chlorhexidine, now I wash myself at home, the holes are delayed. But the question is different, my bite changed)) I began to lisp, and the sharpened 6th tooth in the lower row began to interfere with me - it's hard for me to talk because of it. It seems that it interferes like a bone. I want to cry, I feel inferior. What should I do?
Good afternoon, Oksana. In your situation, you need a consultation with an orthopedic dentist who plans treatment to the end result and the correct bite. It is also necessary to see a dentist surgeon about the holes of the extracted teeth (so that there is no dangerous inflammation).
Violation of diction was manifested due to the removal of 8 teeth. This phenomenon is temporary, the recovery process will occur without additional intervention, although it will take some time, as a result, diction will be restored.
The fact that the 6th and 7th teeth were cut off on the day of removal, I think is wrong, since orthopedic treatment should be resorted to after healing the holes. Perhaps the inflammatory process that you mentioned when talking about the taste of pus formed as a result of foreign particles entering the fresh wound during the preparation of the teeth.
Hello, 5 days ago they removed the wisdom tooth, 38. They removed twice, the first time the upper part in pieces, but that was a month ago. I took a free picture - no roots were visible, made a paid - two roots. They were removed, within five days the place of the tooth and gum with the tonsil hurts. By the way, the roots were removed one by one crochet. It hurts to swallow. Today was at the reception, they said that there are complications. What caused these complications?
Hello, Shakir. It is worth noting the unprofessional surgeon (possibly in combination with outdated diagnostic equipment). Missing 2 tooth roots is almost impossible.
As for postoperative pain, this is a fairly common occurrence, and is determined both by the individual characteristics of the body and the possibility of infection (development of alveolitis). You are shown dynamic observation by an experienced doctor until the pain disappears completely.
Hello! Tell me please. A week ago, periodontitis was treated on the lower right six. After cleaning the canals, put the medicine and put a temporary seal. On the morning of the next day, the cheek was very swollen and swelling appeared under the chin. Temperature, pain when swallowing and shot in the ear. They made an incision - it didn’t help much. We decided to delete. Decided - done. The removal was quick, but the pain in the hole has been preserved for the 4th day, although it is of normal color and begins to drag on. The upper jaw and lower jaw. In the ear, it gives pain anyway, it hurts to swallow. The swelling on the cheek is a little gone, but under the chin it hurts and the swelling remains. I drank the antibiotic Leflock, rinsed with soda. Now doxycycline and rinsing with furatsilinom. I drink painkillers all the time. See a doctor after 4 days. Maybe I should contact you sooner and should I worry about my symptoms?
Hello, Natalia. Yes, in your situation, you should consult a doctor earlier, as dangerous complications are possible - for example, the transition of inflammation to the maxillary cellular spaces. Perhaps, as a result of the unsuccessful treatment of periodontitis, the infection spread to the tissues, plus an injury was caused when the tooth was removed.
So do not wait and endure another 4 days, contact your doctor right away.
Hello. They immediately removed the two lower teeth of wisdom - the pressure was on the seventh, terrible pain (they just got out and removed them). After removal, it hurts for a month, reduces the jaw. Everything hurts. Was at the neuropathologist - diagnoses the trigeminal nerve. A month has passed since the deletion. There is a panoramic snapshot before deletion, is it necessary to do it after deletion and contact the ChLH? Because it seems to me that it's all because of the teeth.
Hello! Pain can be for various reasons, from the parts of the tooth left in the hole (or a cyst left) and ending with the provocation of pain by the sharp edges of the hole under the gum (in this case, gum injury can occur “from the inside” even after a month after tooth extraction) . Since severe pains are felt, it is advisable to take a panoramic picture, as this will give an idea of the condition of the tooth holes, as well as the condition of neighboring teeth. Sometimes it happens that after removal, the hole was sore, then the pain almost disappeared, and after some time (after 2-3 weeks, for example), acute pain occurs associated with the destruction of the seven (six) in which pulpitis or periodontitis occurred . This option should not be excluded until a full diagnosis is made.
Good afternoon, the day before yesterday, the anterior 4 was removed on the upper jaw; the next day, edema formed. There is a gray coating inside the hole. Do not tell me what to do? There is no doctor nearby. I started drinking cyprolet yesterday, 1000 mg per day. Rinse is not much rotokan.
Hello! The best option would be to visit a doctor, since without professional help, alveolitis (if it suddenly arises) sometimes proceeds with complications, and home treatment helps slowly (if at all).
If the dynamics will not improve, then it is better to go to the doctor.In this case, you will need to find out how well the tooth extraction was carried out - the inflammation of the hole is often the result of the roots of the tooth, fragments, granulomas left in it ... So in the absence of a positive effect for 2-3 days, and especially - the general condition worsens and ( or) conditions in the oral cavity, you should immediately run to the doctor.
Hello! 3 days ago removed the bottom 8-ku. There was no pain, as usual. But the wound is very deep, there was no clot either. On the 2nd day in the evening, a little shot in the ear. On day 3, nothing hurts, there is no temperature, something white is going on in the hole, but there were no clots. What could it be? Should I sound the alarm and run to the dentist?
Hello! Most likely, the doctor put a drug in the hole to prevent alveolitis and (or) improve healing of the hole. In general, the light color of the edges of the wound or the bottom of the hole against the background of the absence of other symptoms is the norm at which you should not run to the dentist. In the absence of negative dynamics, it is enough to follow the doctor's recommendations and wait for the full restoration of the gingival crest.
Good day. After removing the 8-ki did not know that you can not take a shower. I barely stopped the blood from my nose ((After the cheek it swelled up within 3-4 days ... A week passed, the gums no longer bother, the swelling disappeared. But every day I spit blood from my nose. It feels like there is always high blood pressure. What is the reason ?! I pulled out a tooth in Nigeria, in the village (although it is difficult to even call this place), and I doubt that there are good specialists in such a hole.
Hello! I assume that you are writing about the removal of the upper wisdom tooth, during the extraction of which there was damage to the wall of the maxillary sinus (maxillary, if in the old way). It is because of this that nosebleeds are possible and not only. I am sure that we need a confirming picture, which is most likely to reveal a damaged wall, or (a little less often), the bottom of the hole communicates closely with the sinus, due to which the hematoma seeps in the form of blood into the sinus in the form of blood from the pressure, from which it enters in the nasal passage.
Regarding bad specialists in Nigeria: this can happen in any country, if you have the anatomy of the upper wisdom teeth has this feature. This is not uncommon, but not very common. Rather, these are occasional cases with any dentist surgeon. Some specialists may experience this more than 10-20 times during the practice, while others - no more than 3-5 cases of the total number of patients (based on 1 thousand patients accepted).
Hello. A week ago, I removed the lower retiniated figure eight on the left. Removal was difficult, the tooth was divided into two parts to pull out. From the next day, the cheek was swollen, sore, the temperature kept at 37.2. At the moment (7 days later), the temperature remains at around 37 in the evening, there is practically no swelling, only a slight swelling of the cheek from the bottom where the tooth was removed. The pain is mild (I have drunk only 2 times of pain medication), but at the same time my tongue hurts on the left with sudden movements, it’s a little painful to chew and open my mouth. In the mirror, the gum is very poorly visible from the other side, but it seems that where the seams and tubercle of the gum are in place of the tooth, either a crease, or a fossa, or a gum sewn together is somehow strange. And with some movements of the tongue, it is as if something is stretching badly. If before opening your mouth wide was not a problem, now the mucous membrane seems to stretch and gives pain somewhere in the palate. All this week I was drinking antibiotics prescribed by the dentist and rinsing my mouth with chlorhexidine. Worried about seams and temperature. Can it last so long?
Hello.The initial stage of healing of the hole after removing the wisdom tooth can last up to 2 weeks - the swelling and hematomas resolve, the pain goes away, the temperature normalizes. However, usually an elevated temperature is observed no more than 3-4 days. In your case, the process has clearly dragged on. This does not mean that something is going wrong - the healing process is different for everyone, but there is reason to still go to the doctor to find the source of inflammation, which causes an increase in body temperature for such a long time. Most likely, the doctor will confirm that the healing of the hole is proceeding normally, however a face-to-face consultation will not hurt - after a complicated extraction of the retained teeth, this is especially true.
Regarding the seams - without inspection, according to the description alone it is difficult to say something. But it’s too early to worry about them - the healing process has just begun, so the discomfort is quite natural.
Goodnight. 6 days ago they removed the horizontal 8. They deleted about 45 minutes, more precisely, two roots: one grew to the tongue, and the other rested against 7. Tapped, tormented for a long time. 7 days have passed, the jaw crunches on this side, in the ear region. What to do? Tell me please.
Hello. During the procedure, excessive pressure on the area of the extracted tooth could lead to an excessive tensile load on the ligaments of the temporomandibular joint (in very rare cases, if the doctor doesn’t perform correctly, the jaw may be dislocated). In such cases, it is necessary to give maximum rest to the joint in the next 2-3 weeks (avoid wide opening of the mouth, exclude hard foods). The situation should gradually return to normal, however, if you notice that this does not happen (there is no positive dynamics), then it is better to see a doctor, as problems with TMJ can lead to a number of complications in the future.
Good day! My aunt was removed 8-ka bottom right. Over the next two days, she was nauseous and lost consciousness several times. They called an ambulance, the doctor diagnosed with vegetative-vascular dystonia. More than two weeks have passed, a wild headache does not go away, only painkillers injections save. They made a circular shooting of the jaw - they say that everything is in order. I went to the manager, the pain in my head subsided a bit, but she still pursues. And with a lower left numbness. Tell me, please, what kind of examination is necessary, what is the reason for this symptomatology? Is the trigeminal nerve damaged? Thank you in advance for your consultation.
Hello. Such a condition could be caused by a general vascular reaction of the body to the stress. Numbness of the lower lip, chin indicates a trauma to the mandibular nerve or its compression by the resulting hematoma. Usually, after removing a wisdom tooth, sensitivity is restored within a period of 1 to 6 months (in very rare cases, when the nerve is seriously damaged, numbness can last for years). To clarify the situation with a long headache, it makes sense to go to 1-2 good clinics (not dental, about the general profile) and get the opinions of different specialists. Physiotherapeutic treatment can also be prescribed there, which sometimes helps with paresthesia, helping to accelerate the restoration of the sensitivity of numbed areas of the face.
Hello. She removed the wisdom tooth, put the turunda, then in the next step she was removed. After I ate, food stuck in the hole. I put water in my mouth and then spit it out. It seems that she cleaned everything. When I did this, I did not wash off the clot! Then, looking at the hole, I saw a bone! This is normal? And can the tooth hole with the food remaining inside be closed?
Hello, Alina. The hole cannot close with food inside.As for the bone - you may have taken fibrin for the bone (this is a white coating that indicates the normal healing process). If you nevertheless rinse out a blood clot covering the wound and thereby expose the bone, then healing can be dragged out without medical intervention (in such situations, alveolitis often develops). Since the situation is not clear, I recommend contacting your doctor in advance to clarify it.
Hello. Tell me, please, what can it be? In May of this year, she noticed an increase in the parotid and submandibular lymph nodes on the right, without pain. After a while, there was a “running” pain in the chewing teeth on the right. I went to the dentist - the pictures showed normal teeth, but since most of the pain was in my lower tooth, the second from the ear, I was treated and filled. They said that it should not hurt. But the pain persisted. I took a panoramic picture, there was visible a retarded wisdom tooth from below. I went to the ChLH on June 17, the tooth was hardly removed, sutured, and drainage was put. Healed all well, the drainage was removed.
After a while, the pain appeared in the first tooth lower from the ear. I went to the dentist again. I was told that everything was fine there, cleaned the stones. They said that if it hurts, go to a neurologist. And indeed, the pain has returned. I went to a neurologist. She confirmed that after tooth extraction, the nerve may hurt, prescribed a treatment that included dexamethasone. I was treated. During the treatment, nothing hurt and everything was fine. But a week passed, when I stopped being treated, the pain returned, but it became different. The treated, sealed second tooth lower from the ear hurts, and the bone under it hurts. There was a restriction on the opening of the mouth (not strong). Tell me what should I do? Thank you so much for the answer.
Hello Valeria! Your case is far from standard. First you need to conduct a thorough examination and collection of anamnesis, and additional research methods will also be required. Only after this is it possible to more accurately make the correct diagnosis. Based on the complaints described, it’s still hard to even figure out which specialist should treat you. Perhaps several specialists should help here. I recommend that you consult an experienced dentist with all the extracts and previously diagnosed diagnoses and tune in to a thorough diagnosis.
Good afternoon! About a month ago, the lower right 8 was removed. The roots were at an angle, but there were no difficulties. 3 days after the removal was at the doctor’s appointment, everything is fine. About a week after the removal, a strong throbbing pain began, sometimes she could not sleep. I came to the doctor in a week. As a result, everyone cleaned and washed with chlorhexidine, put the medicine and a sponge. The pain stopped. After that, she was still 2 times at the doctor, changed the medicine and the sponge. A week after the last appointment, at which the doctor said that the wound was clean and healed well, I saw something like a blood clot and some kind of yellowish plaque. When pressed, pus comes out, but there is no smell, pain and temperature, too. I made an appointment with a doctor. But while I wait, you can go crazy. What could it be?
Hello. Judging by your description, there is no longer an inflammatory process, since the temperature is normal and you have no pain. As for the "yellowish plaque" - this is fibrin, which forms at the site of a blood clot over time. A normal phenomenon, as well as the allocation of a sacrum, which you, most likely, took for pus. You write that the liquid comes out when you press on the blood clot - you should not squeeze anything, so you can only harm the healing process. So be patient and show yourself to the doctor at the appointed time.
Three weeks ago, I removed the lower chewing tooth (more precisely, its root). A few days later, the alveolitis began. When I got to the doctor (after a couple of days), I realized that there was a fistula on the inside. They cleaned my hole, laid a turunda with medicine, and told me to come to my doctor in a couple of days. By the way, they took a picture - there were no roots. But at the bottom there was something white, in the examination room it was suggested that this granuloma comes out. Prescribed ciprolet.
I came to the doctor two days later. She cleaned the turundo, put some fiber there too. Two weeks after that, the same fistula was filled with pus. Inadvertently poked him with a toothbrush. Rinsed with an antiseptic, but after a couple of days a new fistula came out. I’ll get to the doctor only three days later, by that time it will already be a month after tooth extraction. I am very worried that the consequences will be difficult, with difficulty reversible. There is no pain, the gum reddened around the fistula. Is it osteomyelitis? What should a doctor do in such cases?
Hello Yulia! Osteomyelitis is a very long process, usually accompanied by pain, bad breath, fever, and general malaise. Judging by your descriptions, it does not look like osteomyelitis. However, for making an accurate diagnosis and assessing the severity of the situation, just a description is not enough - additional research methods are needed (preferably computed tomography of this area and examination by an experienced dentist surgeon is required). If necessary, re-inspection of the well and conservative therapy will be necessary.
Was at the doctor’s picture. It was embarrassing that a shapeless dark spot appeared that did not connect anything to the hole of the extracted tooth. He was not there before. The doctor did not give me a clear answer. In general, he believes that everything is fine, but through the fistula he nevertheless cleaned (everything was already overgrown from above). Alveogles laid in this hole. Antibiotics prescribed only local. Around the wound, everything turned white, but I hope it goes away. After removal, the incisions also turned white. I do lotions with iodinol. To my question about osteomyelitis, the doctor said no, it's not him. I felt the walls there, everything is dense. And I have a fear that this spot in the picture is pus, I am very afraid to start it.
Regarding osteomyelitis - thanks for reassuring.
Hello. 10 days ago, removed the lower right 8. There was no clot. Since the pain didn’t abate, I did an x-ray - a fragment of a tooth remained in the hole. They cleaned it, drank cyprolet for a week (500 mg 2 times a day). There is no temperature, I eat normally, but a yellow coating is visible inside the hole. What could it be? And is it worth going to the doctor? Thanks.
Hello, Dilya! The yellow color in the hole is usually due to stained fibrinous plaque, and this is the norm in wound healing. The absence of pain, fever, and putrid odor from the mouth indicates a normal healing process.
Hello! Please help me with advice. 4 days ago pulled out a molar tooth (lower, 2 on the right side). The doctor found it difficult to remove, from the third time he was able to remove, and then in parts. He said that 3 roots, it was difficult. They put turunda, let the ice hold for 20 minutes. After I came home. It was very painful, the first two days I could not open my mouth. Turunda is still standing, and there is pain. Every 4 hours I take religion. There is a little swelling and a lump outside. They said to rinse furatsilinom and drink anti-inflammatory. But the 4th day still the pain does not go away, and I don’t like the view from the inside - the place of removal is as if cut.
Hello. Unfortunately, pain after complex tooth extraction does not pass quickly. Continue to rinse and take anti-inflammatory drugs as prescribed by your doctor.However, if the pain builds up, a temperature will appear (and also if the pain lasts longer than 2 weeks), you should consult a doctor to examine and evaluate the situation. Despite the fact that the wound at the site of the tooth seems deep, the mucous membrane is quite quickly restored, and after a while everything will return to normal.
Good afternoon. After removing the 6-jaw, the jaw ached for about 5 days. A week and a half passed, now it does not hurt. At the very beginning, after the extraction of the tooth, the bite changed - it began to lisp, whistle, the jaw moved sideways to the sensations. If you push a little on the opposite side, then the bite returns to normal, and there is no lisp. Also, the ear was slightly blocked from the side on which the tooth was removed. The doctor does not see any abnormalities. Tell me, what could it be?
Hello Andrey! During tooth extraction, there is often strong mechanical pressure on the jaw, which can lead to a slight sprain of the joint from the side of the extracted tooth. Usually in such cases, it is recommended to exclude solid food within 1-2 weeks. If during this time there is no positive dynamics, then you should consult a doctor (and it’s better to go to another one, that is, not to the one who says for the current state that he “does not see any deviations”).
Good afternoon! Removed the upper tooth of wisdom, quickly, painfully after almost none. Immediately the temperature rose, kept for 2 weeks in the region of 37-37.4. I felt some kind of patient, there was no pain in the hole, the neighboring teeth ached for a couple of days, then stopped. Then the upper and lower jaw (gums?), Sometimes even the cheek, began to itch in periods. The beginning to periodically crush the temple from the side of the extracted tooth. I noticed that the soft tissues inside the mouth swelled from the side of the removal, but not where the hole is, but where the jaws join.
I went to the doctor who removed the tooth twice, he said that everything was normal, the hole healed perfectly. The temperature did not drop. I went to another dentist, he said that everything looks decent. Prescribed antibiotics for temperature, smear swollen tissue with a metrogyl. The temperature dropped, and I began to feel better, although the temple still sometimes pressed and the gums itched. I finished the course of antibiotics - the temperature is now 36.6, but it immediately seemed to get worse - the temple sometimes presses and even stronger, for some reason it shot into the cheekbone a couple of times while compressing the jaw from somewhere on the upper jaw. Sometimes, a short time, as if an ear hurts. All pain is not strong (except for the shot one), but unpleasant. I make baths with chamomile, smear with gel. What should I do? Do a hole audit? Take a picture? I'm afraid of osteomyelitis. I followed all the recommendations of the doctors, I didn’t rinse the clot, he was in place all the time.
Good afternoon, Irina! The situation you described does not fit the symptoms of osteomyelitis - most likely, your problem is associated with alveolitis. Pain in the temple and ear may persist for some time after tooth extraction. Treatment in the absence of inflammation does not require a hole. Dynamic monitoring by the attending physician is necessary. Therefore, observe with him, and if there is no positive dynamics, then it is necessary, together with the doctor, to think about further actions.