
Most people turn to the dentist for emergency care just for the simple reason that they did not pay enough attention to caries, considering it a kind of “annoying misunderstanding” that could well wait until there was free time for his treatment. As a result, most often acute pain is no longer caused by caries, but by pulpitis, which is associated with damage to the soft tissue inside the tooth. Moreover, often the symptoms of pulpitis continue to be confused with caries, hoping once again to wait or drown out the pain with painkillers.
But the defeat of the pulp chamber of the tooth is far from the limit. The result of excessive “patience” is often the transition of pulpitis to the more difficult to treat diseases - periodontitis. Often the outcome of pulpitis complications is tooth extraction, after which displacement of adjacent teeth, malocclusion, normal chewing of food, and sometimes stomach and intestinal diseases can occur.
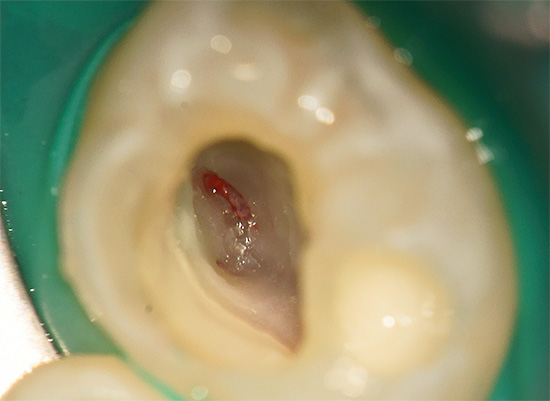
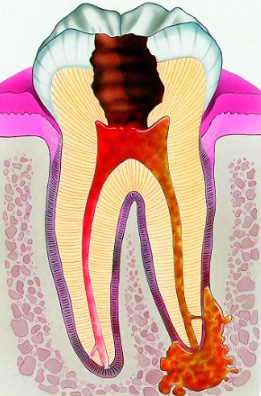
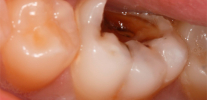
The photo below shows a tooth in which deep caries led to the development of pulpitis:

Many people know firsthand about the possible appearance of the so-called "flux" (periostitis). But few people know that flux on the gum often appears after prolonged pulpitis pain and is the result of the death of the “nerve” in the dental canal with the formation of pus, which simply has nowhere to go, and therefore it goes to the side of the tooth root, inflating the gum.
Over time, the flux can turn into a fistula (see photo):

What is pulpitis, what are the causes of its occurrence, what can it endanger a person’s health and what types of this pathology are there - all of this will be discussed later.
It is interesting
The pain that can occur when exposed to the "nerve" of the tooth was known long before the advent of modern dentistry. During the Inquisition, the first primitive hand tools were used for torture (something like a drill), which, when rotated, crumble enamel and dentin and reach the soft tissues inside the tooth, thereby causing their irritation and destruction.
Of course, everything was done in order to cause unbearable pain in the subject, and it came to a loss of consciousness and pain shock. Then the sufferer was brought to his senses in order to continue exposure to the pulp. Sometimes the torture lasted more than one day, and a person died from a traumatic shock.
So what is pulpitis?
Pulpitis is an inflammatory reaction of pulp tissue (dental "nerve"), which occurs in response to an irritating factor, external or internal. Pulp is a soft tissue pierced by vessels and nerves. There are a lot of nerve cells inside it, which is why toothache is considered one of the most powerful.
Pictures of tooth pulp:
Why does pulpitis cause such severe pain?
Due to the fact that the inflammatory reaction has a phase of edema, during the increase in pulp in size, compression of nerve cells occurs with the development of severe unbearable pain. At acute pulpitis the pulp is covered with a thin layer of carious tissues, and in chronic forms, when the pain is not so pronounced, most often the bottom of the carious cavity communicates with the pulp chamber. In such cases, the pain is aching and becomes pronounced only when irritants get into the "hollow" of the tooth (hot, sharp), or due to a complete blockage of the hole over the pulp with something (seeds, nuts, apples).
As a result of edema and compression of the entire connective tissue bundle, a gradual necrosis (necrosis) of the "nerve" occurs.


In one form chronic pulpitis only the coronal part of the tissue dies, and in the canals it partially remains alive.
Causes of Pulpitis
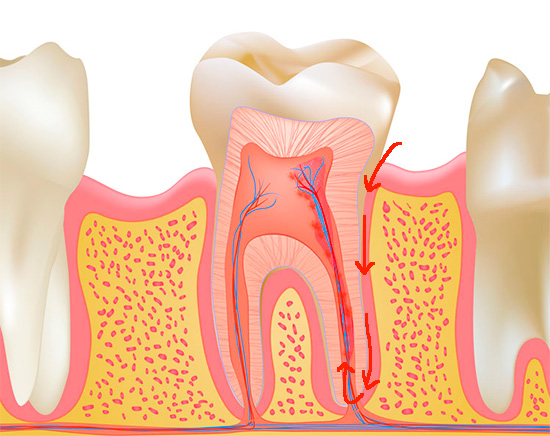
The most common cause (etiology) of pulpitis is deep caries. In the process of deepening the carious cavity, direct or indirect penetration of microbes into the pulp tissue occurs. With direct access, the infection goes directly to the opened pulp, and with indirect access, through the dentinal tubules penetrating the thickness of the dentin.
In dentistry, several methods of pulp infection and pulpitis occur:
- through a tooth crown (caries complication)
- through the opening of the apex of the root with the manifestation of retrograde pulpitis.
The retrograde form of pulpitis is a rare occurrence due to its specific developmental mechanism (pathogenesis). The causes of retrograde pulpitis are:
- Hematogenous (through blood) infection of the tooth pulp with common infectious diseases (flu, rubella, etc.), when the infection spreads to the maxillofacial region.
- When the infection spreads from the infectious foci closest to the tooth roots, which most often become the maxillary sinus with sinusitis.
- Through an infected periodontal pocket (the space between the root and the gum), when due to violation of the gingival attachment, the infection rushes to the top of the tooth root, causing pulpitis.
Also, one of the most common causes of pulpitis is the doctor’s mistakes or his wrong actions. Most often this is due to overheating of the tooth during its processing (preparation), accidental opening of the pulp chamber followed by permanent filling, as well as improper turning of the tooth under the crown with non-compliance with the technique and without the manufacture of protective caps after the procedure. A pulpit tooth begins to manifest itself immediately or after a medical error, often forcing the doctor to redo the entire work again.
It is interesting
One of the rarest pulpitis is traumatic and calculus pulpitis. Injury due to impact, bruising, and falling is most often characteristic of the front teeth: it is in such cases that pulpitis is of non-infectious origin. The resulting symptoms of pulpitis of the front teeth are no different from the "classic" options for the development of pathology.
With calculus pulpitis in the dental "nerve", disturbances occur due to denticles and petrificates - deposits consisting of salts (mainly calcium compounds). These calcified calculi compress the delicate pulp tissue, causing pulpitis.
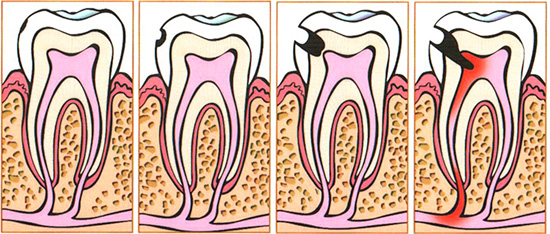
The following picture schematically shows the classic development of pulpitis - after deep caries:
Acute and chronic course of the disease
Pulpitis of the tooth, as a disease, can have several currents: acute, chronic and in the acute stage. Most often, acute pulpitis is first formed, and then chronic. At some point in time, the chronic form enters the stage of exacerbation.
However, this scheme does not apply to all cases: it also happens that the tooth does not acutely ache, and the pathology immediately passes into a sluggish chronic form. Often, a person does not even have exacerbations, when the chronic form of pulpitis smoothly passes into another disease more difficult to treat - periodontitis.
The pathogenesis (development) of pulpitis is directly related to the etiology (cause) of its occurrence and may have its own specifics, however, any inflammatory tissue reaction has much in common. Regardless of what causes pulpitis (infection, trauma, or toxic effect on the “nerve” of the filling material), serious structural changes occur inside the pulp tissue:
- pulp edema;
- blood flow disturbance;
- oxygen starvation of cells;
- difficulty in removing toxins;
- phenomena of necrosis (necrosis).
Among acute pulpitis, focal and diffuse are distinguished.In both cases, the pulpitis tooth hurts not only spontaneously without irritants, but also in the presence of them (sweet, cold, etc.). Night shooting pains and short intervals between attacks, when a person does not feel pain, are characteristic.
The difference between acute diffuse pulpitis and focal pulpitis is the spread of pain along the branches of the trigeminal nerve: pain can be given to the temple, ear, to the infraorbital region, to the back of the head, to the cheekbone, etc. In such cases, a person cannot accurately indicate to the doctor the tooth causing the suffering, and additional diagnostic tools must be used.
With focal pulpitis, the pain is localized in one specific tooth, and the patient is able to precisely point to it.

The consequences of irreversible disturbances in the pulp of the tooth can be chronic forms of pulpitis: fibrous, gangrenous and hypertrophic. The names themselves speak for themselves:
- at fibrous pulpitis degeneration of the inflamed nerve tissue into fibrous tissue occurs;
- at gangrenous - there is gangrene or necrosis of the coronal or partially root tissue inside the tooth;
- with hypertrophic pulpitis, hypertrophy (proliferation) of soft tissue occurs, which often can occupy the entire carious cavity - the so-called "wild meat".

Chronic pulpitis usually manifests itself only as aching pains and weak sensitivity to irritants (especially hot ones). Pain can have an individual duration, often recurring for several months with varying frequency.
As a rule, certain triggers (stress, hypothermia, flu, etc.) lead to a decrease in the body's defenses with the development of the stage of exacerbation of chronic pulpitis, when the whole story with acute pain is repeated again, bringing new suffering.
Feedback:
“I don’t like going to doctors, so I waited. A tooth was terribly sick for several days, I had to swallow pills, and then, lo and behold, the tooth stopped hurting! I even thought - well, it’s necessary, has everything resolved, and now it’s not necessary to make an appointment with a doctor. And then in a week I felt something on the gum above the sore tooth, such as a sore, and her taste was so nasty. Purely intuitively guessed that this pus was coming out. In general, it was not without a doctor - everyone drilled me there, cleaned the canals, there was already a dead tooth. ”
Maxim, Novosibirsk
Pulpitis development options for different groups of teeth
Pulpitis can develop on any tooth, but there are certain groups of teeth that are most often prone to such a lesion. The first place in the frequency of occurrence is occupied by the first molars or, otherwise, sixth teeth, which appear among the first (at 6 years old) and are located in the most unprotected zone, often still having deep and closed fissures (fossae). When spots appear in these areas in the child, the parents do not immediately understand what it is, but with the deepening of the process every day approaches the moment when the child begins to complain of severe spontaneous pain in the tooth - this is already pulpitis.

From the front teeth, pulpitis most often develops on the central and lateral incisors. Fangs are the least susceptible to caries due to its massiveness and structural features.
The lower front teeth, as a rule, are all the least susceptible to the development of caries and in the future - pulpitis due to the high degree of washability by their saliva. Since saliva is a kind of “liquid enamel”, it is in this group of teeth that lost mineral components (calcium, phosphorus) return more quickly.
However, one should not forget that despite such “luck” of the lower front teeth with regard to the risks of developing complications of caries (pulpitis and periodontitis), the lower teeth are more prone to deposit tartar on them precisely because of the same highly saline saliva ( see the example in the photo).

The most dangerous complications of pulpitis
The most dangerous complications of pulpitis occur against the background of prolonged patience of pain or regular taking painkillers. Most often, after pulpitis, acute or chronic periodontitis develops - inflammation of the tissues around the root.
In the acute form of periodontitis, in most cases people go to the dental clinic for the reason that there are very strong throbbing pains and it is simply impossible to touch the tooth, sometimes even the tongue. Often, when this happens, the body temperature rises and there is a feeling that the tooth “grew”. If a doctor is consulted precisely at this stage of the process, then after treating the tooth and penetrating into the area where the pulp should be, plentiful pus with an unpleasant odor comes out of the canal.

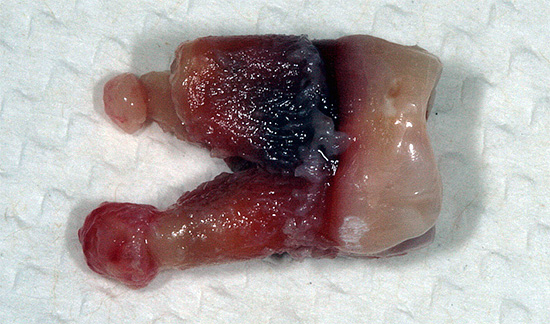
In chronic forms of periodontitis, the most unpleasant formations on the gum are fistulas. These are channels that depart from the inflamed root of the tooth and from which a badly smelling pus periodically comes out, making it easier for a person to suffer.
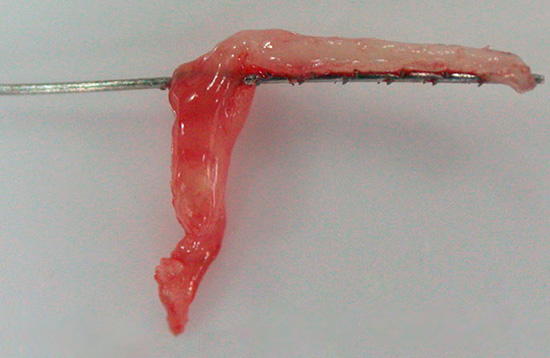
The most difficult to treat and hazardous to health is chronic periodontitis associated with the so-called cysts. Some people are well aware of the possible growth of tissues around the root in the form of granulomas and cysts, as they saw this picture after removing their tooth. These "purulent sacs" on the extracted teeth hang from the roots, having a color from red to cyanotic color. This picture leaves no one indifferent and is remembered for a long time.
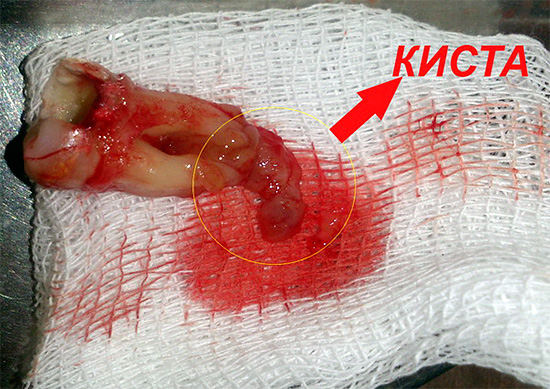
Read more about the formation of a cyst on the root of the tooth, its health hazard and possible complications when removing read in separate article.
If you thought that this “horror” ends, you will have to disappoint. The above complications of pulpitis were the most “peaceful” ones, which most often lead only to tooth loss, but there are diseases that affect the general health of a person: periostitis, osteomyelitis, abscess, phlegmon, sepsis.
Periostitis is an inflammation of the periosteum of the jaw amid the spread of pus under it. As a result, the well-being worsens, the temperature rises to high values, the shape of the face can change, there is a feeling of fullness in the gums near the diseased tooth. Often after these severe conditions, a person more than once regrets that he did not cure on time a relatively harmless pulpitis.
Osteomyelitis - melting or dissolution of the bone, when the purulent process covers the jaw spaces so much that, in addition to the diseased tooth, neighboring teeth begin to stagger.
On a note
With the prolonged development of osteomyelitis, a person can seek the help of a dentist-surgeon to eliminate the source of infection, but the result of the removal of a diseased tooth can be a fragmentation of the jaw along with it or a fracture. Since in the process of osteomyelitis progression the bone becomes less durable due to its “dissolution”, even a small effort often leads to injuries of varying severity.
An abscess (limited purulent inflammation) and phlegmon (diffuse purulent inflammation) are diseases that develop amid complications of pulpitis and often lead to death of a person. They are associated with the active germination of the focus of infection in the spaces between the muscles, where there are vital formations (vessels, nerves).
In the photo below - phlegmon:

Sepsis is the infection of the blood with toxic products of infection, leading to intoxication of the body, a violation of its protective forces and, ultimately, sometimes to death.
How to recognize pulpitis on your own
In order to prevent serious complications in time, it is useful to be able to independently recognize pulpitis at the very first symptoms. Diagnosing yourself is not so difficult.
When toothaches occur, you should first of all understand their nature: with caries there is no acute spontaneous pain, it appears only from external irritants. In acute pulpitis and its exacerbation, there are both of these signs.And with acute periodontitis, the tooth most often cannot be touched at all, your well-being can worsen, hot sharply intensifies the already unbearable throbbing pain.

Chronic pulpitis is more difficult to detect, but if it is possible to inspect the carious cavity, pulpitis becomes easier to recognize. If some kind of soft tissue occupies the carious cavity, then most likely chronic hypertrophic pulpitis develops. If a long aching pain occurs when food enters the tooth, then the opened nerve is highly likely, as in fibrous or gangrenous pulpitis.
Chronic periodontitis has much in common with chronic pulpitis, but only with chronic forms of periodontitis can there be fistulas on the gums near the diseased tooth. Only with periodontitis, the gum near the tooth can “swell”, hurt, pus is often released from under it.
Despite the possibilities of self-diagnosis, only a dentist can make a final diagnosis by performing a set of diagnostic measures (examination, palpation, percussion, thermometry, EDI, radiography).
The photo below shows a visiograph for radiography:

Pulpitis treatment and prevention
After determining pulpitis, the doctor draws up a plan for his treatment. There are 3 approaches to the treatment of pulpitis: with the preservation of the entire "nerve", with its partial removal, with the complete extraction of the pulp from the system of equine canals.
The first way to keep the entire pulp in a viable state is currently not popular due to frequent complications, so doctors usually prefer the latter option. Partial pulp removal is also used, but only when there is no way to go through the entire channel due to its complex structure or the presence of foreign bodies in it.

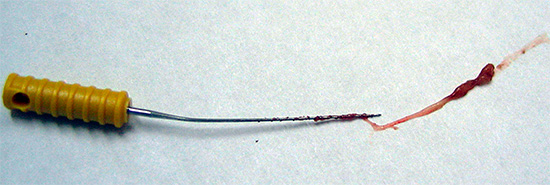
The main importance in the full treatment of pulpitis is the good drug treatment of the canals and their filling to the physiological apex (apex). To do this, anesthesia is necessary, the channels are processed with special tools similar to needles (files), washed with antiseptic solutions and sealed with hardening pastes with or without gutta-percha pins.
On a note
Often, treatment of pulpitis takes from 1-2 to 3-4 visits. This is due to the approach to treatment, with or without the use of pastes for necrotizing the "nerve" (arsenic or not containing arsenic), with the setting of special antiseptics or drugs for additional channel disinfection, designed for several days.

For more information about the interesting nuances of pulpitis treatment, see the article Modern methods of treating pulpitis.
Fine there should be no pain after pulpitis treatment. With restrictions, the presence of post-filling pains after treatment is allowed for no more than 5-7 days, which are manifested only by discomfort when biting on a tooth (especially solid food).
In order to prevent the development of pulpitis, timely treatment of tooth decay that occurs on the tooth is important. This is a minimum program. As for the maximum program, prophylaxis should be started even before the onset of caries, and follow the recommendations aimed at strengthening the teeth and protecting them:
- To clean with toothbrushes and pastes of all accessible surfaces of the teeth every time after eating;
- To clean zones of spaces between teeth with flosses (flosses);
- Do not abuse sweet;
- Conduct professional hygiene once every six months (cleansing of plaque and stone);
- Perform remineralizing therapy and deep fluoridation of all teeth in consultation with the dentist.
The implementation of these recommendations will not only allow you never to feel the horror of pulpitis pain, but also protect your teeth from the development of caries.
Interesting video about pulpitis
And here is the treatment of pulpitis
Root canal treatment


Very useful article. Thanks!
Thanks for the useful information.
I am terrified, I want to go to the dentist!
What a horrible picture boy.
Yes, I also finished badly with painkillers, then half cheeks swollen + pus removed with its root and septum. Take care of your teeth from a young age, and 2 times a year to be checked by a doctor!
Tomorrow to the doctor!
Yes toothache - it's scary, I also took a ticket for Tuesday. Tooth ache for a week, just in my pulpit, this is not a joke.
Thank you for the article. Very helpful. Already run to the dentist, you never know)
It is written in plain English without any scientific terms. Thanks.
Yes, the trouble is our fear. But at the moment, medicine has become successful and pain-free dental treatment, I am very happy about that. More and depends on the doctor, I got a great therapist, cured 11 teeth, and there was no pain.
The therapist does not treat the teeth, can only give direction.
Thank you for the article with clear illustrations. Now I understand very well what is going on with my teeth. And when everything is clear, it’s easier to make the right decision and not wait for the alleged “self-passing”.
Well, how to do so, so as not to hurt the teeth ...
Pull out.
Yesterday I was at the doctor's office, removed the inflamed nerve, cleaned the three channels and put a temporary seal. Free, by policy! Thanks to the doctor and many years of healthy life!
I have, it turns out the pulp. Insert the seal, they said that it is necessary to finish the cure. Well, let's hope that everything will be fine.
Thank you for the article. For unknown - worst of all)
Thanks, good article. Now I treat tooth, but, unfortunately, the pulp. I will never again drag out a visit to the dentist, and to hell with work, because of which there is no time to get to the doctor. And damn, sweet, however, very much affects the teeth ...
Horrible. Urgent to the dentist.
I recently treated all teeth are very grateful to our doctors. Take care of your teeth.
I could not stand such a terrible picture!
Before reading, I do not think that will be all serious, in a complex level. Now, I understand that tomorrow I have to go to the doctor ...
Thanks! A very useful and interesting article.
Half of the face was very painful. We put trigeminal neuralgia. The treatment failed. Signs as in the pulp. We must go to the dentist. How to distinguish between diseases?
Hello! It is important to assess the integrity of all teeth - search for causal tooth is defined as the pain sensations (where "shooting" pain), as well as its appearance, which can vary due to the destruction of tooth decay. You did not write about whether an X-ray or panoramic radiography was performed. Whatever it was, in your case it requires a thorough diagnosis.
In the meantime, I note only a couple of points for reflection.Trigeminal neuralgia is characterized by: a sharp paroxysmal pain that occurs when eating food, talking. Pain does not occur at night. There is an increased sensitivity during palpation of the skin at the places where certain nerves exit the bony holes of the skull. But with pulpitis (diffuse, which is manifested by irradiating pains), on the contrary, often pains appear at night, and there are “suspicious” teeth in the oral cavity, which often have broken surfaces. In addition, with pulpitis, there are no pains confined only to communication with people when there is an active facial expression.
So you should definitely go to the dentist.
Thank you very much for the helpful information!
I went to the doctor with a complaint of tooth pain. Took a picture. There were no visible violations, and the doctor advised me to buy fluoride toothpaste and massage the affected tooth with the paste. A month later, she was forced to consult a doctor again. The result is pulpitis! Treatment: either paid (at least 8,000 rubles), or can be removed. Here is a doctor’s advice!