Often, teeth begin to hurt at the most inopportune times - many people are well aware of this from their own bitter experience. Often the symptoms of pulpitis are taken by surprise during long holidays, at work, on vacation, and it is not always possible to immediately consult a doctor for help. It is impossible to guess at what point deep caries, as the most common cause of pulpitis, is complicated by inflammation of the tooth “nerve” with the appearance of characteristic symptoms, this can happen at any time.

It is important to keep in mind that in case of untimely treatment at the clinic, pulpitis often goes into purulent formswhen it is possible to endure tooth extraction and expensive prosthetics, or even processes irreversible for the general health of a person, sometimes bordering on life and death.
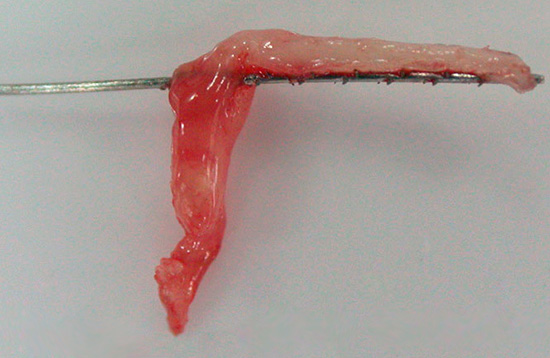
The photo below shows a tooth removed due to complications after pulpitis:

But how to distinguish the signs of pulpitis from other diseases of the tooth (say, from severe pain with deep caries), which complications can threaten and whether there are ways to prevent them - this and much more will be discussed later.
Pulpitis characteristic as inflammation of “living” tissue
In order to better understand the root causes of the various symptoms of pulpitis and to imagine in advance what may await you during future treatment, you must first understand what, in fact, inside the tooth can actually hurt. The very definition of pulpitis greatly clarifies this issue.
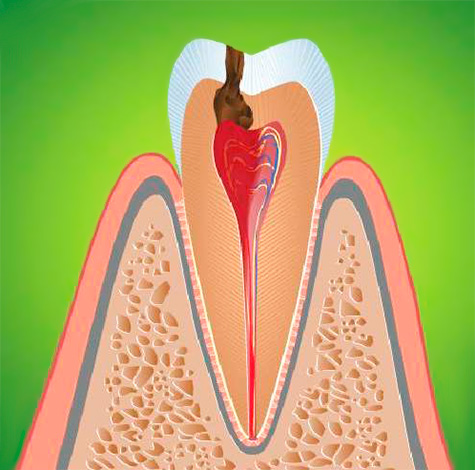
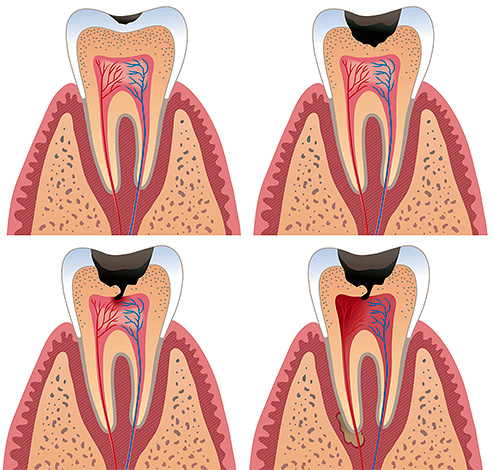
Pulpitis is an inflammatory process that occurs in the so-called pulp chamber, or, otherwise, in the dental “nerve” (neurovascular bundle). And this process is associated in most cases with the activity of microorganisms: as a result of untreated deep caries, pathogenic microflora sooner or later penetrates through the thinned dentin into the soft tissue of the pulp with the appearance of characteristic signs of tooth pulpitis.
Inflammation in the pulp proceeds according to the same laws as in any other tissue. Against the background of the aggressive effects of bacteria and their toxins on living tissue, a gradual death of cells occurs, which activates inflammation factors. If we could observe this picture under a microscope, then its meaning would be as follows:
- immunity sends cells (leukocytes) to fight the infection to destroy the source of pulp damage;
- the result of this struggle are structural changes in the pulp tissue, up to its complete necrosis (necrosis) and the appearance of a characteristic clinic of chronic or acute pulpitis.
Soft tissues inside the tooth cannot recover on their own, but the process can go into a long chronic process with limited inflammation from surrounding tissues - this helps protect them from spilled purulent fusion.
In the picture below, this process is shown schematically:
Question: Why does pulpitis sometimes cause a strong bad breath?
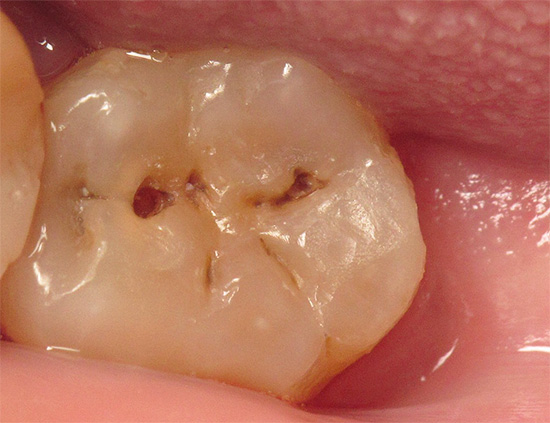
With a deep carious process, food particles accumulate on the walls and bottom of the carious cavity, and often there is practically no self-cleaning of the cavity or it is very weakly expressed. The result of the gradual decomposition of organic residues is the appearance of a putrid odor from the mouth - this symptom often accompanies deep caries. Moreover, if pulp necrosis occurs, then the smell of the rotting tooth “nerve” in the pulp chamber also joins the smell from rotting food debris. And the more carious cavities (especially with pulpitis), the more pronounced are the signs of bad breath, which interferes with normal communication with people.
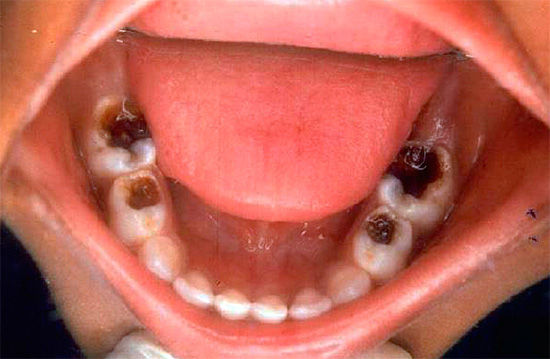
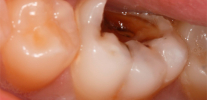
A photograph of a tooth with a deep carious cavity, which at any moment can cause pulpitis:

Classic pulpitis symptoms
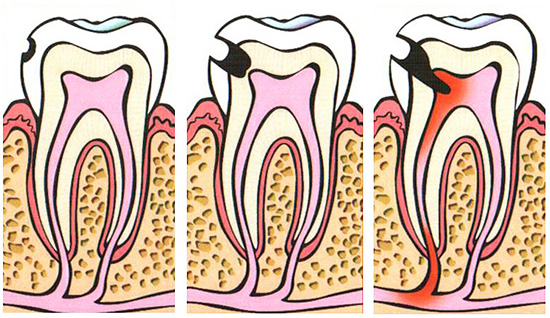
There are many pulpitis classifications, but the simplest one to understand is the one that most dentists use to correctly make an accurate diagnosis and determine a treatment plan. According to this classification, all pulpitis is divided into acute and chronic.
Acute pulpitis is of only two types: focal and diffuse, and chronic - three: fibrous, hypertrophic and gangrenous. There is also a category of pulpitis in the stage of its exacerbation.
A characteristic symptom of acute pulpitis is spontaneous paroxysmal pain, often occurring at night, which often lasts 2-3 weeks in duration. With these forms of pulpitis, the dental “nerve” remains covered with carious tissues, and there is no external communication with it. The pain is intense: it is cutting, shooting, tearing, brings severe torment, often causing painkillers to be used.
The appearance of pain symptoms in acute pulpitis is also provoked by external irritants (cold, hot, sweet), but unlike caries, such pains do not persist for a long time even after the elimination of such an irritant.
The fundamental difference between acute focal and diffuse pulpitis is determined by the characteristic clinic. In acute focal pulpitis, you can accurately indicate a bad tooth, and during diffuse pulpitis, the pain radiates (gives) along the branches of the trigeminal nerve. For example, from the lower teeth, pain is directed to the ear, back of the head, and even to the temple. The patient’s upper tooth “shoots” into the zygomatic region, into the region of the superciliary, often the pain radiates to the opposite jaw.

Chronic pulpitis often occurs, bypassing the acute stage. Almost always pains are aching in nature, and often such pulpitis can occur even without symptoms.
Chronic fibrous pulpitis has symptoms characterized by aching pain when eating hot and solid foods. An asymptomatic course is also characteristic of this variety. Sometimes with fibrous pulpitis, the pulp chamber is opened, that is, it communicates with the oral cavity.
Chronic hypertrophic pulpitis is extremely rare, mainly in pediatric dentistry. The main clinical signs of this pulpitis is the growth of pulp due to the formation of new tissue or, as it is called, “wild meat”. However, often the entire cavity is occupied by this tissue, which causes pain when eating, especially hard.


At chronic gangrenous pulpitis Symptoms depend on whether the pulp chamber is closed, where the tooth pulp is located, or has already been opened. When the chamber is closed, the pain is very pronounced, can even be spontaneous, but more often - strong aching from the hot. With an open cavity, gangrenous pulpitis gives a blurry clinic, so the final diagnosis can only be made at the dental appointment.
Question: Is there a temperature with pulpitis?
Most often, there is no elevated temperature with pulpitis, and this symptom characterizes more periodontitis, periostitis and other complications. However, in some cases, immunity can respond with a slight increase in temperature within the low-grade (37.0 ° -38.0 °), especially in children. Most often, temperature can occur when signs of pulp necrosis appear (chronic gangrenous pulpitis).
The photo shows a tooth “nerve” extracted from a pulp chamber:
The main difficulties of diagnosis and the devices used in this
To diagnose pulpitis, you should contact your dentist for a series of additional tests. In addition to studying the symptoms of pulpitis, the following methods are also used:
- The so-called objective method using a dental mirror and probe;
- Thermometry;
- Instrumental diagnostic method (EDI);
- X-ray diagnostics.
Almost 70-80% of information about the form of pulpitis of the tooth can be obtained on the basis of an assessment of symptoms and a study of the carious cavity when examined by a dental mirror and when probing. An objective study allows us to distinguish pulpitis from deep caries, various forms of periodontitis, etc.
Probing allows you to understand whether the pulp chamber of the tooth is opened, whether it is painful to probe, whether the opened “nerve” bleeds, if the tooth itself is discolored, is there pain in it when percussion (tapping the tooth with the blunt end of the probe handle) - all this also has importance for making an accurate diagnosis and subsequent treatment.

From the practice of the dentist
Based on the symptoms and the appearance of the carious cavity, an experienced dentist can make a preliminary diagnosis of pulpitis and even determine its type, which in practice is not of fundamental importance (except for gangrenous forms of pulpitis, which require special drug treatment of the tooth canals). In order to prove the presence of a carious cavity with the pulp chamber, dentists of the old school can probe with great force, causing sharp pain when the tip of the probe gets into the tissue of the still dead pulp. Such methods of differential diagnosis due to the not very humane approach are not acceptable in modern dentistry.
A commonly used diagnostic method is thermometry. This is a test of the reaction of a tooth to cold and hot. If the tooth pulp has already died, the tooth will not respond to cold water. The reaction to temperature stimuli with pulpitis is more pronounced than with caries, and does not last long after the elimination of the temperature stimulus.
EDI or electroodontodiagnosis. Perhaps this is the most informative method in such a diagnosis, allowing not only to distinguish pulpitis from other tooth diseases (caries, periodontitis), but also pulpitis among themselves (acute types of pulpitis, chronic). Its principle is based on the use of devices that can act on the tooth with weak electric currents. At the same time, a healthy “nerve” reacts with insignificant pain sensations even at a current strength of 2-6 μA.

With a painful reaction to a current of such strength, they are diagnosed with caries. The exception is deep caries, when the tooth may begin to respond to a current of 20 μA. In any case, pulpitis, as a rule, react to currents above 20-25 μA. And the occurrence of a reaction at 100 μA already indicates the complete death of the pulp and the occurrence of periodontitis. Acute forms of pulpitis respond to currents up to 40-50 μA, and chronic ones up to 90-100 μA. Gangrenous pulpitis in the destruction of the coronal part of the nerve is determined at a current strength of 60-80 μA.
X-ray diagnostics - is a fairly informative method. For example, by the nature of the change in the structure of the bone around the root (s) of the tooth, we can understand that we have signs of pulpitis, and not periodontitis, we can also determine approximate borders of the carious cavity and suggest a violation (opening) of the pulp chamber. This is important to confirm or refute the diagnosis of deep caries.
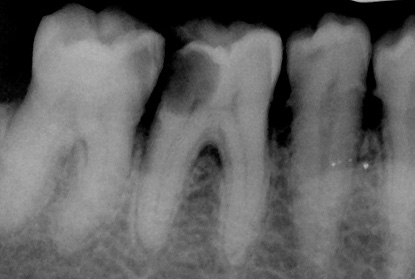
In chronic forms of periodontitis, as a rule, changes in the bone tissue around the root are significant, and in acute pulpitis there are no such changes at all (with chronic gangrenous pulpitis a slight expansion of the periodontal gap is sometimes possible).
Symptoms of rare types of pulpitis
Traumatic pulpitis. It differs from the classical forms of pulpitis in the cause of the appearance: the neurovascular bundle is damaged due to a tooth injury. As a result of the traumatic factor, tooth inflammation begins, sometimes with the addition of infection from the oral cavity.
Despite the possibility of infection, in their pure form, such pulpitis is non-infectious, but it causes quite typical clinical symptoms: severe pain from irritants (cold, hot), as well as spontaneous and paroxysmal pain. Traumatic pulpitis is common in childhood and adolescence, as well as in asocial categories of the population.

Retrograde pulpitis is a rare form of pulpitis, sometimes causing confusion at the dentist's appointment when there is no carious cavity, and pulpitis symptoms (bouts of pain, night and long pains) are present. In such cases, the infection inside the tooth enters through the hole at the top of the root.

Common causes of retrograde pulpitis are:
- Sinusitis
- Periodontitis
- Osteomyelitis
- Actinomycosis
and etc.
Concrete pulpitis is also a rare form of pulpitis, in which there is no infectious factor in the development of spontaneous or prolonged aching pain in the tooth. Inflammation of the pulp develops as a result of prolonged compression by calculi - parietal deposits present in some people in the dental canals.
Most often in old age, the lumen of the channels is narrowed by denticles or petrificates - salt deposits. The clinical signs of calculus pulpitis are often blurred: there may be prolonged aching spontaneous pain, or only from irritants (hot).
Note: How to find a bad tooth with retrograde or calculus pulpitis ...
Unfortunately, in most clinics there is no EDI that allows you to check which teeth are healthy and respond to a current of 2-6 μA, and which sick tooth is already 20 μA and above. X-ray diagnostics can sometimes help only with calculus pulpitis, where areas with signs of channel blockage by salt accumulations are detected. Almost always, the bone tissue around the root with pulpitis is not affected.
Large dental centers and research institutes have equipment for EDI, and in most clinics they can search for a causative tooth based on complaints from the patient, the pulpitis clinic, but in fact, using the “poke” method, when the patient can partially help the doctor by pointing out a rough tooth. Sometimes 1-2 healthy and “innocent” teeth are treated at the same time, but it is worth emphasizing the moment that for any doctor, a meeting with retrograde or calculus pulpitis is a very rare phenomenon that may not occur at all during his practice.
Signs of dangerous pulpitis complications
Complications of pulpitis can occur as a result of the lack of treatment of the tooth, or its inappropriate conduct. The first category of cases occupies the main position according to statistics, since long-term local infection in the "nerve" of the tooth sooner or later passes into a purulent process, which often causes serious complications.
Among these quite often occurring complications include:
- Periodontitis is an inflammation of the tissues surrounding the root of the tooth (the ligamentous apparatus that holds the tooth in the socket), which is manifested more often by a purulent process with enlargement and swelling of the gums near the diseased tooth or the appearance of fistulas on the gums, from which pus flows into the oral cavity.
- Periostitis, also called by the people "flux". This is an inflammatory process under the periosteum of the jaw.
- Osteomyelitis is a purulent inflammation that develops already in the bones of the jaw itself, most often against the background of untreated periostitis.
- An abscess is a limited purulent inflammation, accompanied by fever, intoxication of the body and serious consequences.
- Phlegmon is a very formidable complication of an abscess, when a purulent infectious process spreads through the tissues of the jaw, soft tissues of the face and can cause death.
- Sepsis - against the background of reduced immunity, high aggressiveness and the spread of infection in the jaw, intoxication or infection of the whole organism with severe consequences can occur.



In this case, the list of pulpitis complications is not complete, but even it makes it clear how dangerous it is not to treat pulpitis at the first sign of its appearance.
After treatment of pulpitis, complications sometimes occur, especially when contacting low-budget organizations with unskilled and inexperienced doctors, but they are not as massive as the first category of complications.
Question: Why are canals easier to treat with pulpitis of the upper front teeth?
When symptoms of front tooth pulpitis appear, most people turn to the dentist for help. Since all the upper front teeth from canine to canine have only one, most often wide canal, in almost 100% of cases there are risks of complications during and after treatment of tooth pulpitis minimized. Usually, canal treatment takes 2 times less time than intracanal treatment of the posterior teeth (they have many roots, and the percentage of complex canal anatomy is high).
See for example interesting nuances of the treatment of pulpitis in three-channel teeth.
First aid for pulpitis pain
If the symptoms of tooth pulpitis interfere with work or rest, but it’s difficult to get to the dentist in the next day, then it’s not forbidden to help yourself by choosing either folk methods for getting rid of pulpitis painor medications.
Common folk methods:
- rinsing the oral cavity with warm decoctions of chamomile, St. John's wort, sage, oak bark, mint, lemon balm, valerian - until the attack disappears completely or its acuity is significantly reduced;
- rinse with warm soda-salt solutions (usually a teaspoon of soda and salt is diluted in a glass of warm water);
- rinse your mouth with vodka or hold it near a diseased tooth for a while. This method of treatment has age restrictions.

Common medications to relieve pain symptoms of pulpitis:
- Use regular pain medication for oral administration (Ketorol, KetanovPentalgin, Nise, Dexalgin and others) in therapeutic doses. Before taking them, you should consult (can be remotely) with a therapist or dentist, as side effects, contraindications or individual intolerance are possible.
- Alcohol tinctures of eucalyptus or valerian. They are suitable both for applications and for the treatment of the carious cavity. In this case, a certain anti-infective and analgesic effect is achieved.
Often, propolis is also used to close the carious cavity with an open "nerve" as a temporary filling. If there is no allergy to this drug, then for temporary use it is perfect.
And finally, the tip: Is it possible to warm a tooth when the first signs of pulpitis appear?
In acute toothache, it is not recommended to warm the sore spot outside. A warm heating pad, scarves and warming compresses stimulate inflammation, translating it into a purulent process in just one night. Heating always exacerbates the infectious process, which can not be said about the warm rinses of the oral cavity itself. Therefore, it is not necessary to apply the sick cheek to the battery to reduce pain - the opposite effect is obtained.
Interesting video: treatment of pulpitis under a microscope
What is important to know about pulpitis


Thanks for the detailed description of pulpitis.